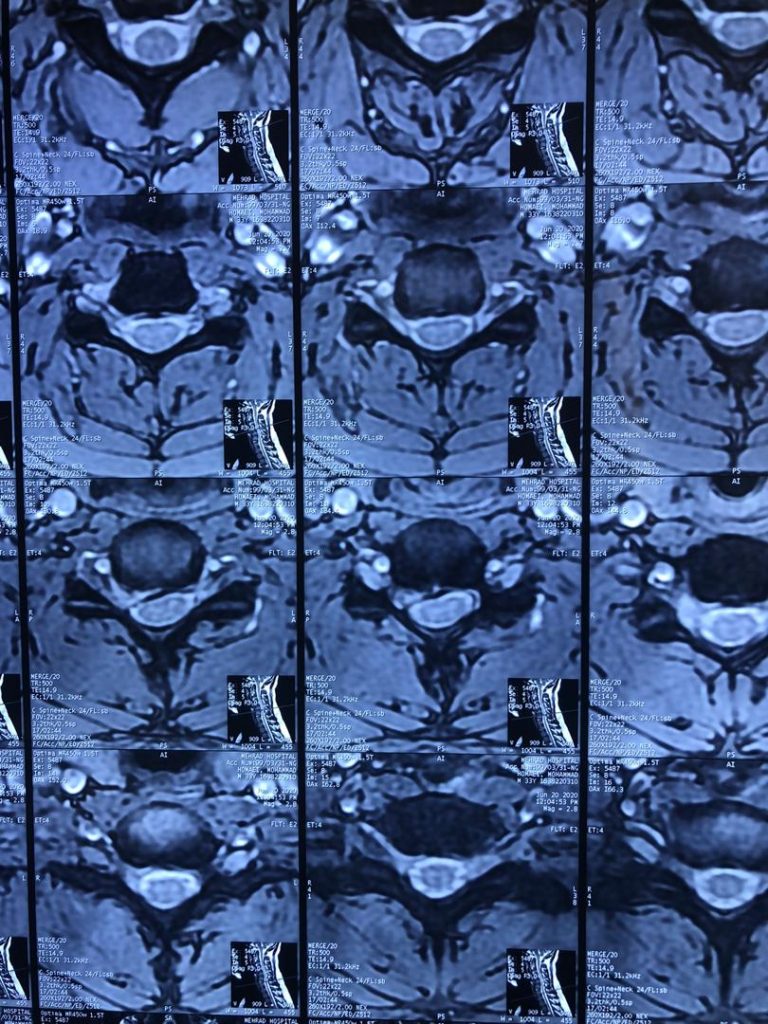
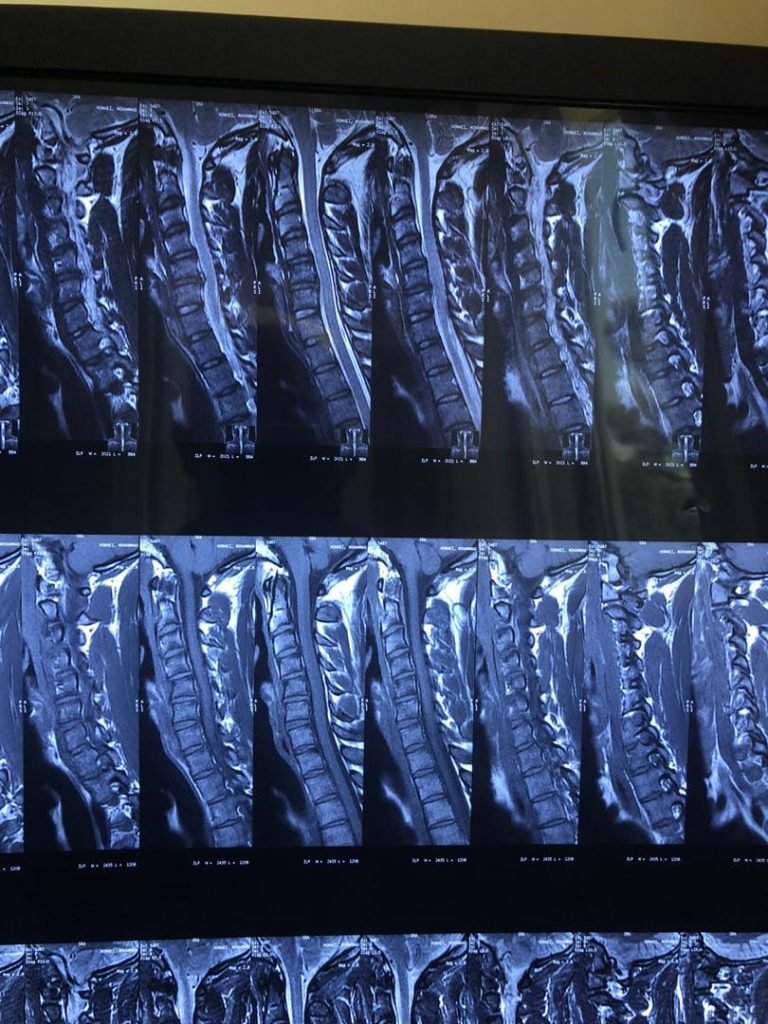
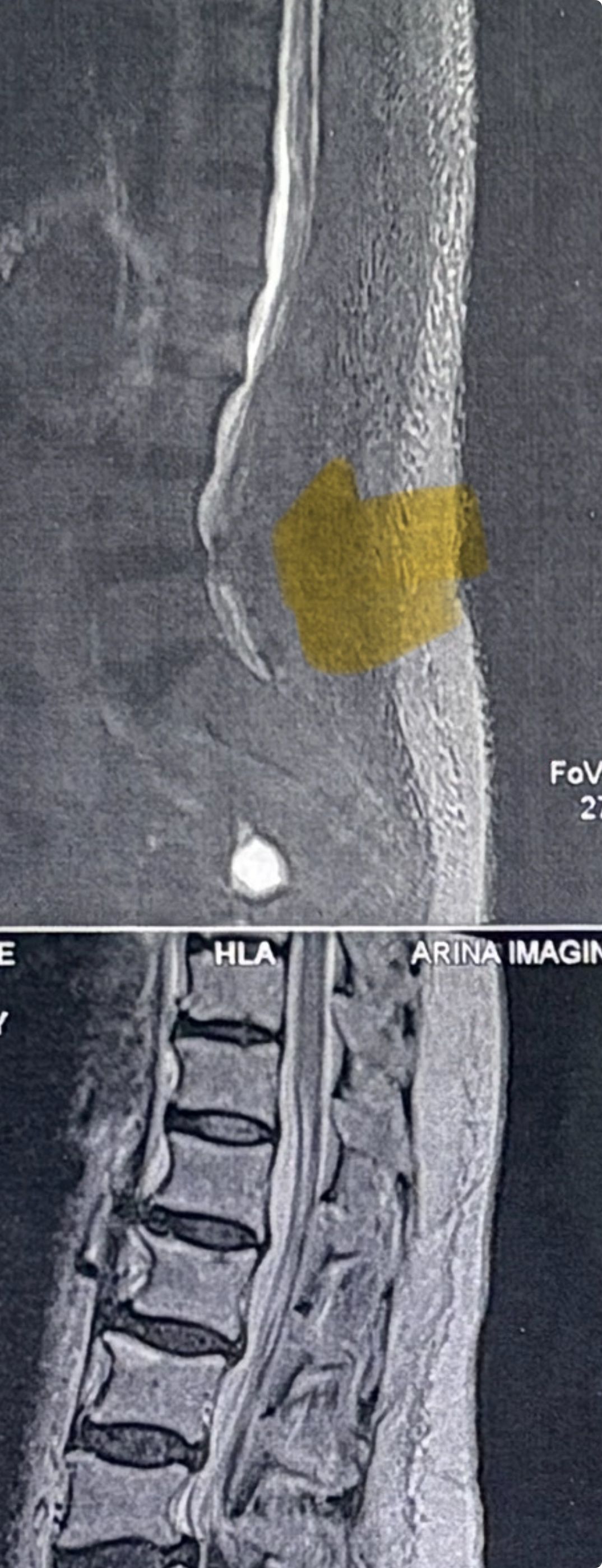
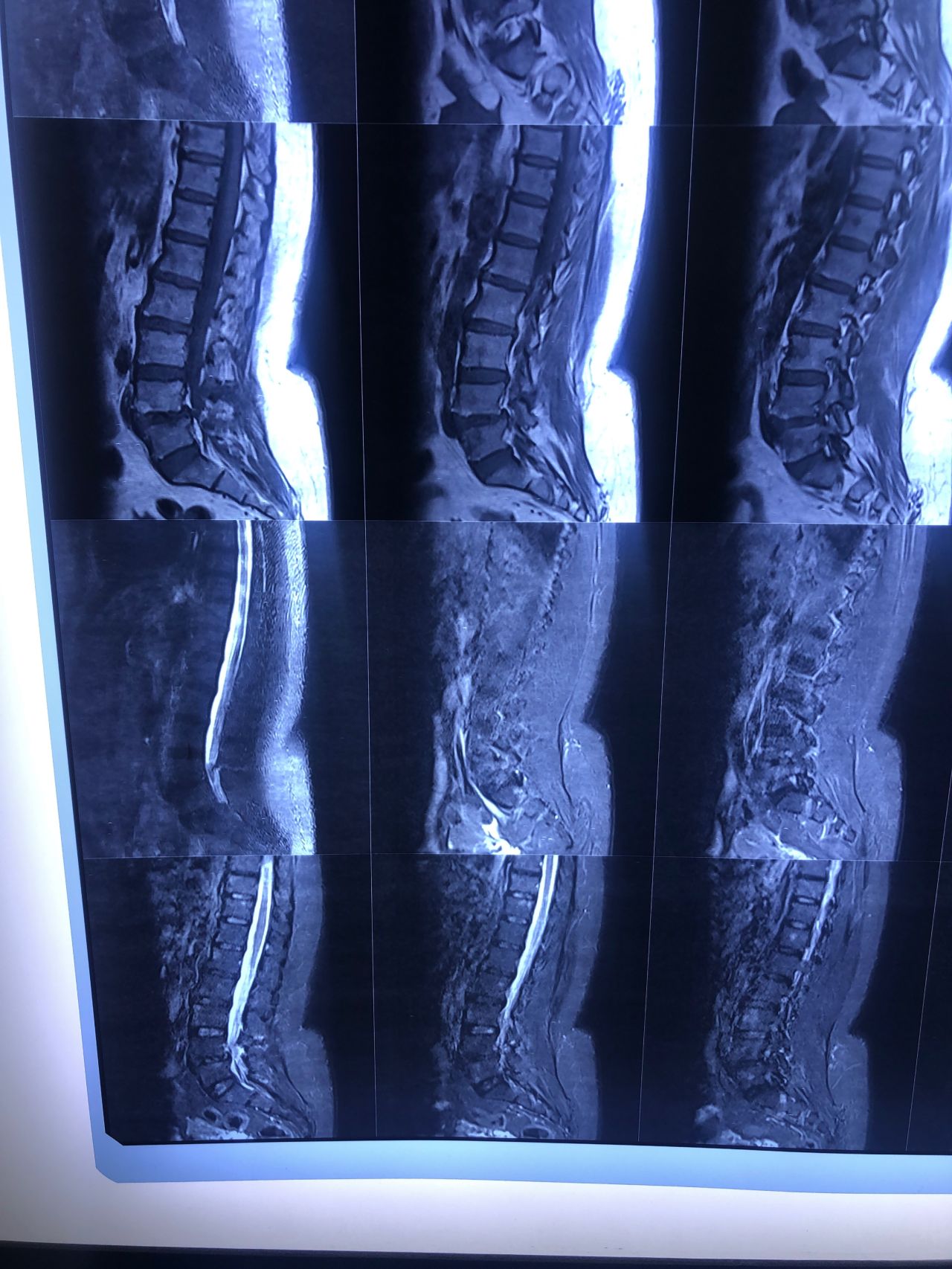
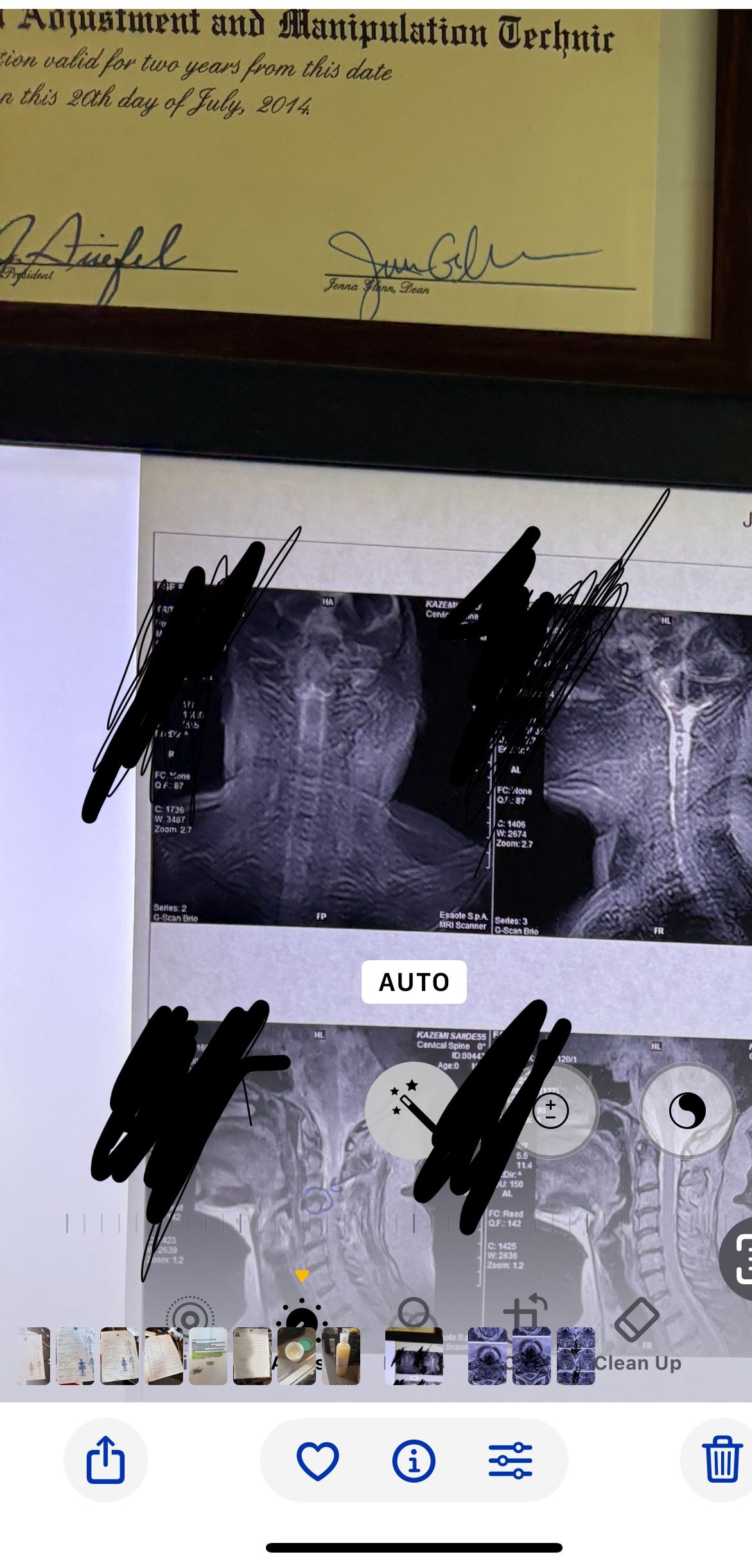
MRI before/after chiropractic treatment by DR. Cyrus
MRI of patients who have improved after chiropractic treatment by DR. Cyrus Salimian
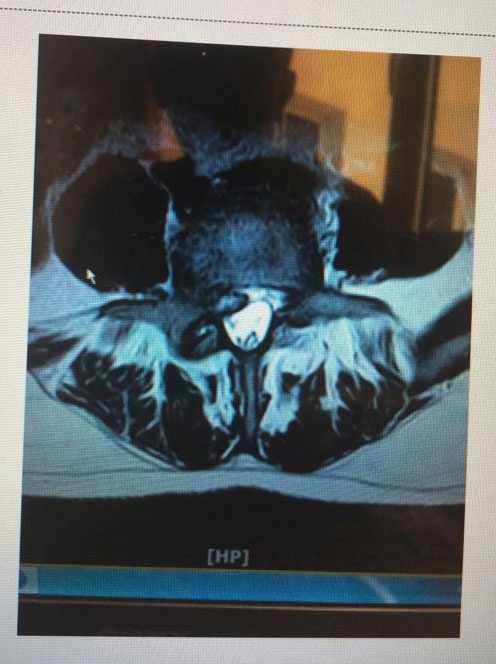
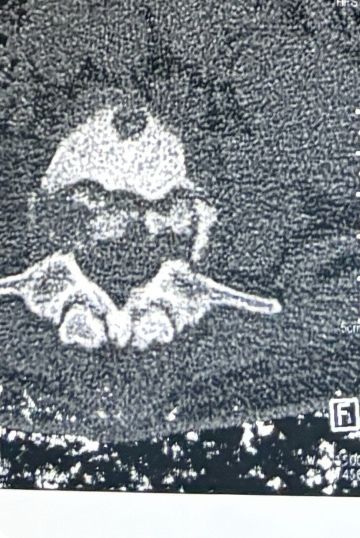
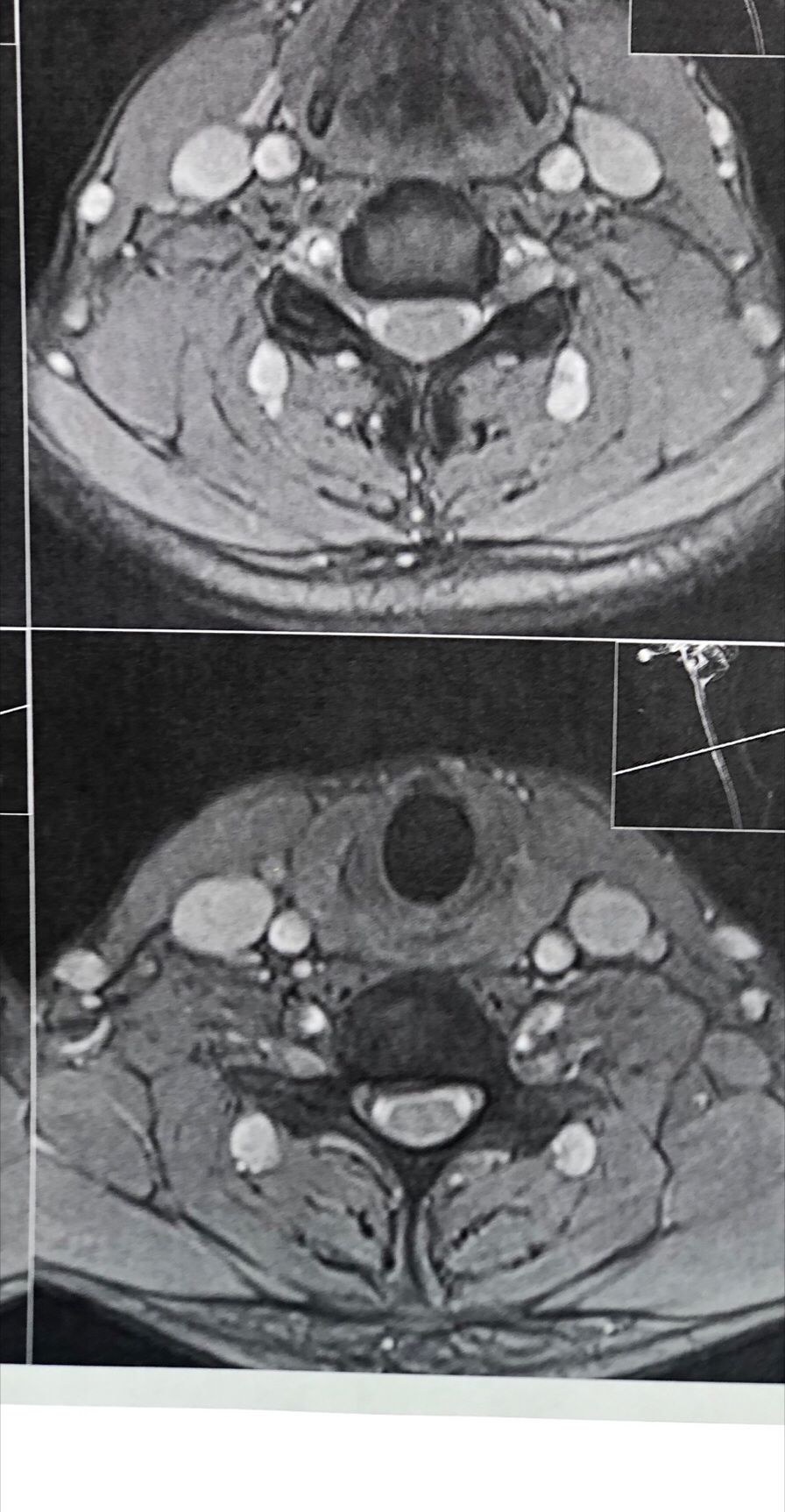
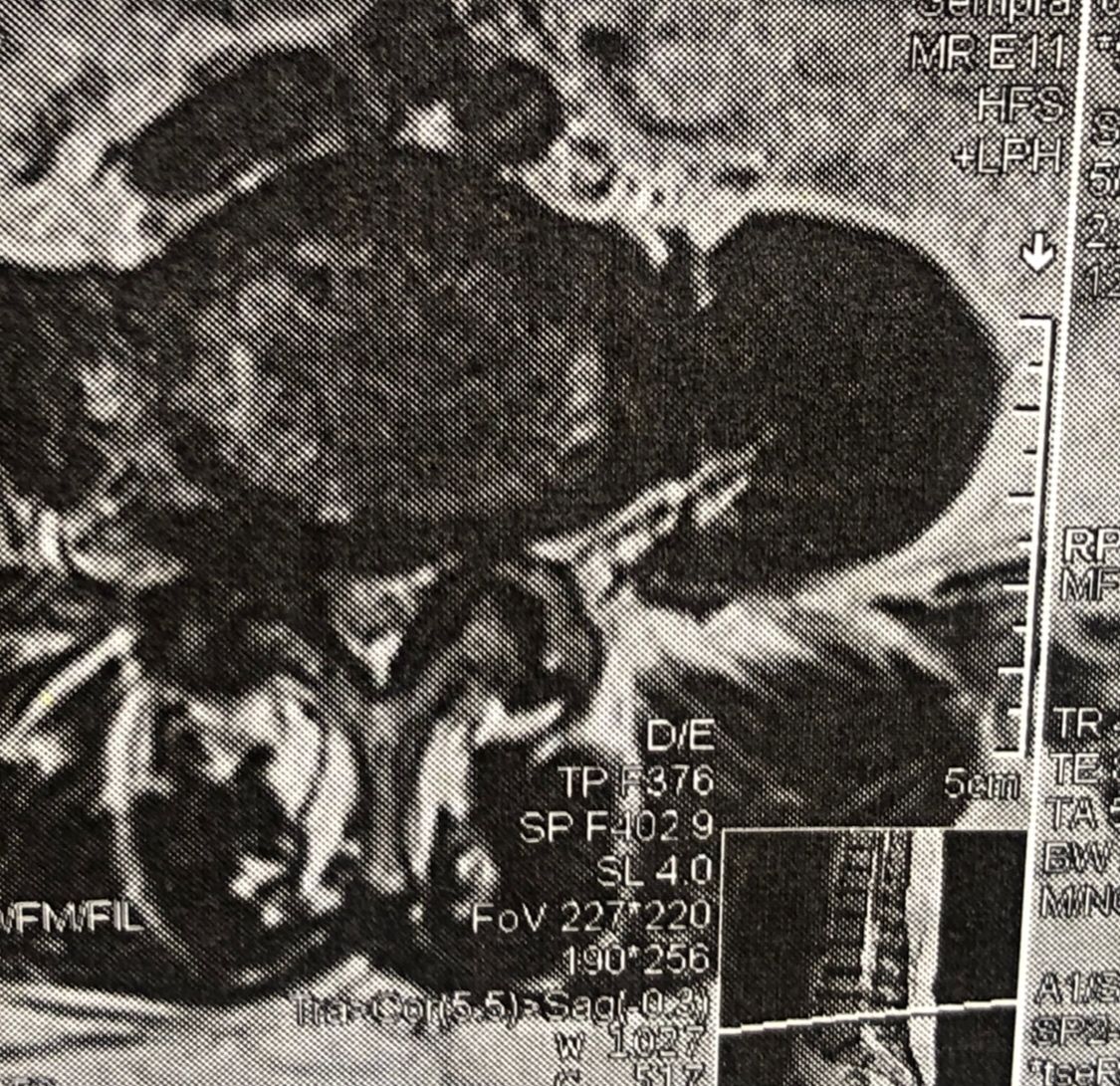
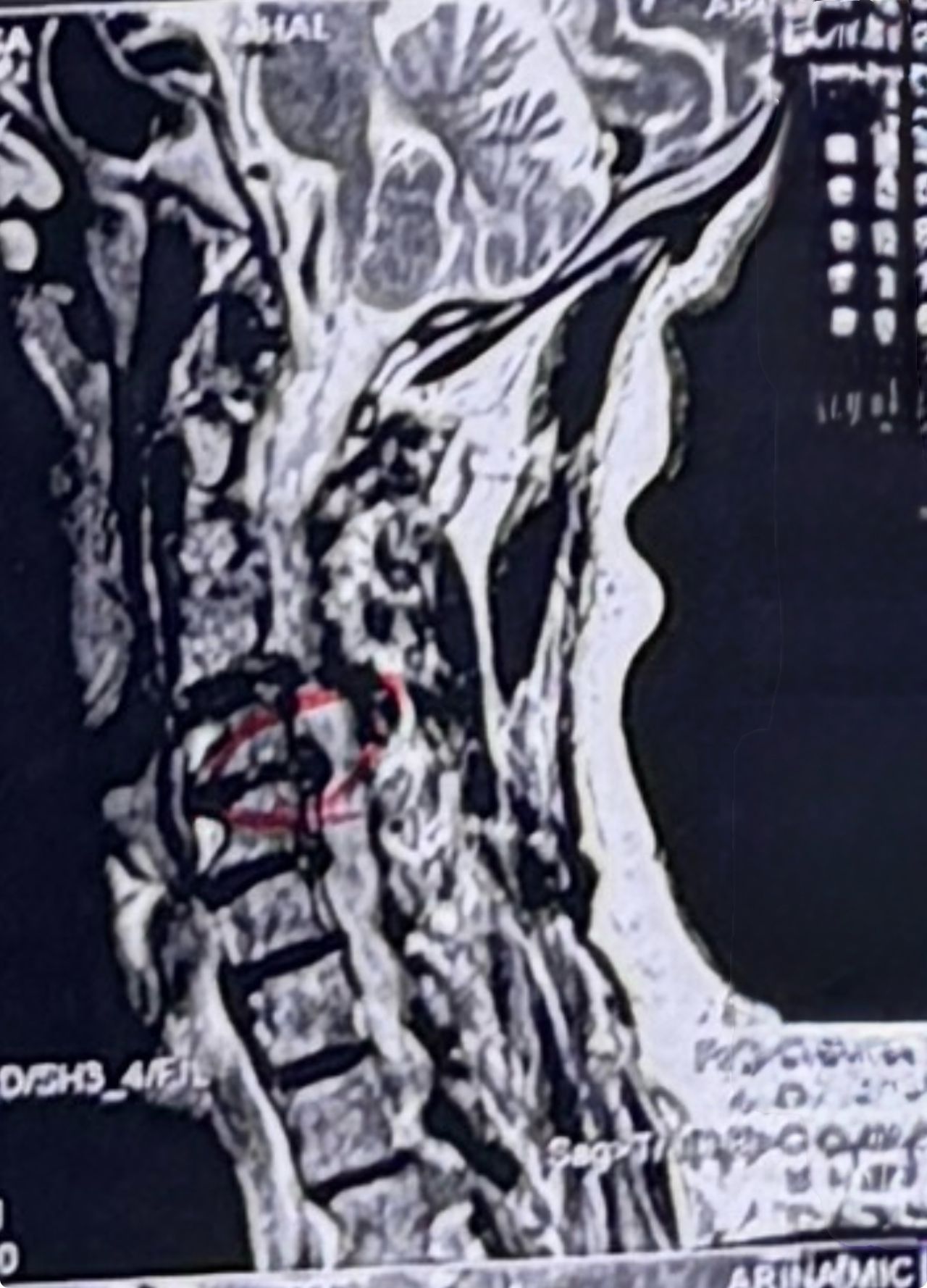
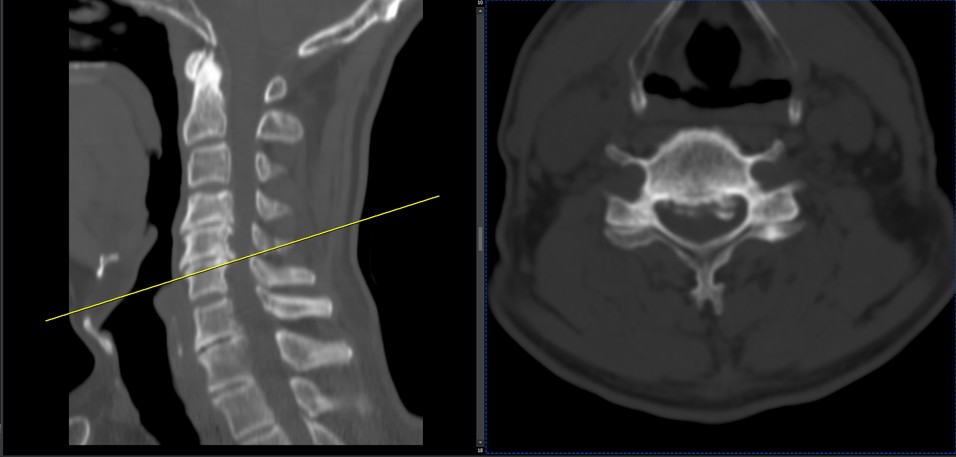
Case 1
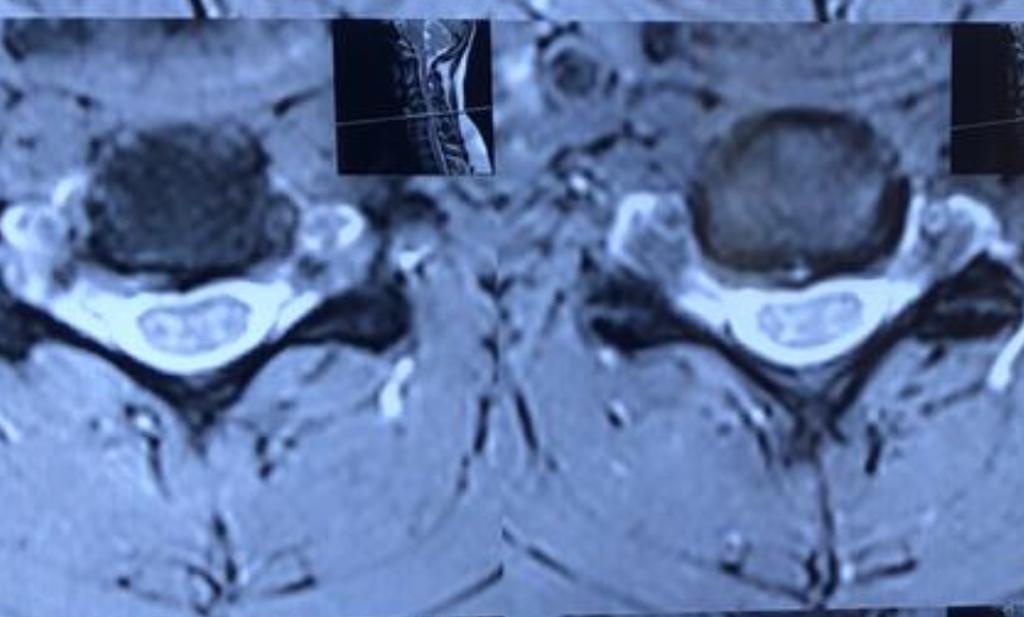
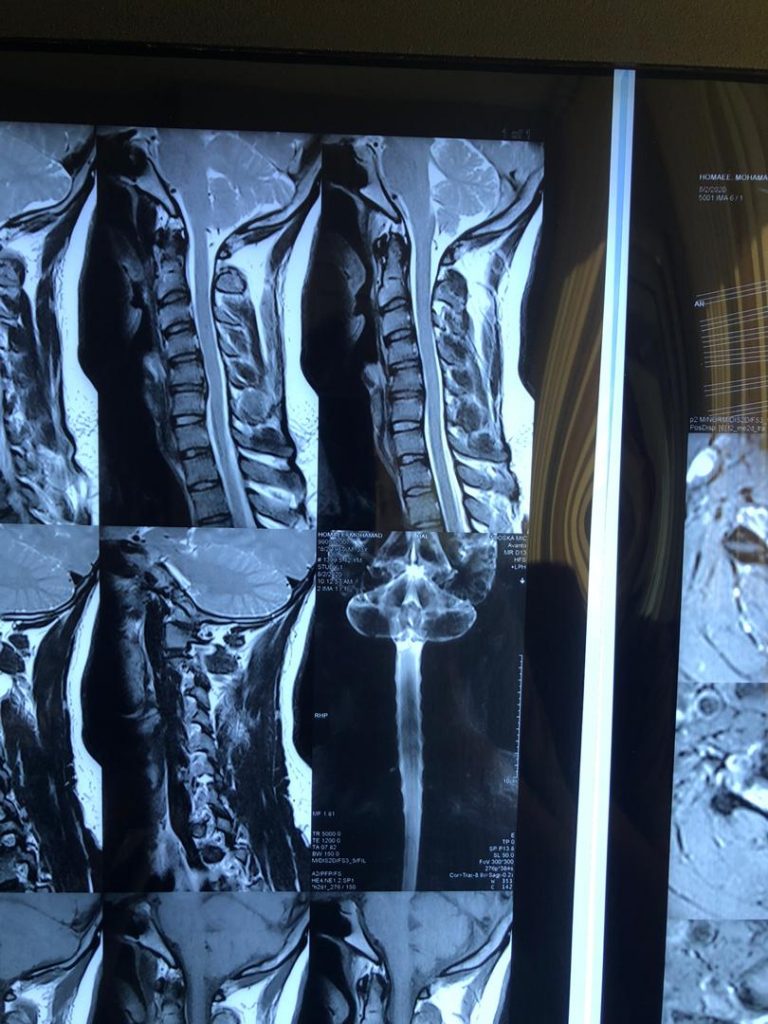
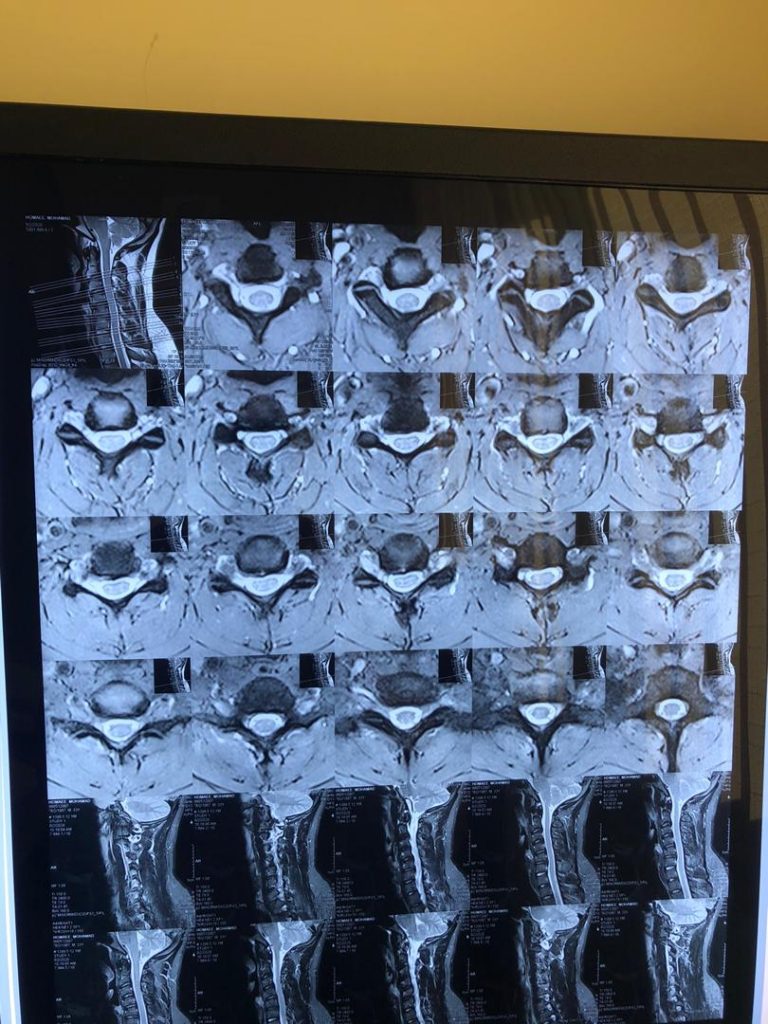
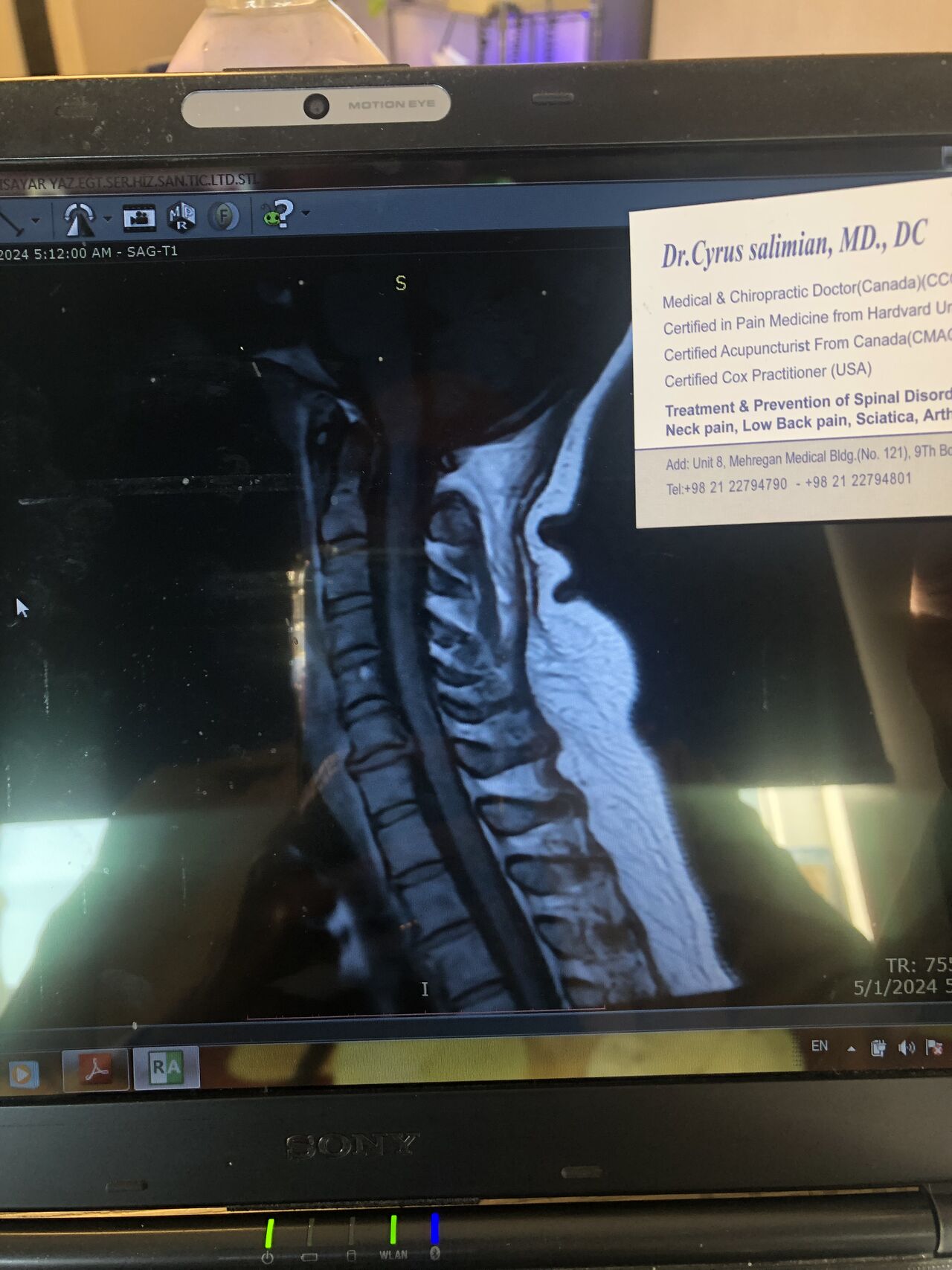
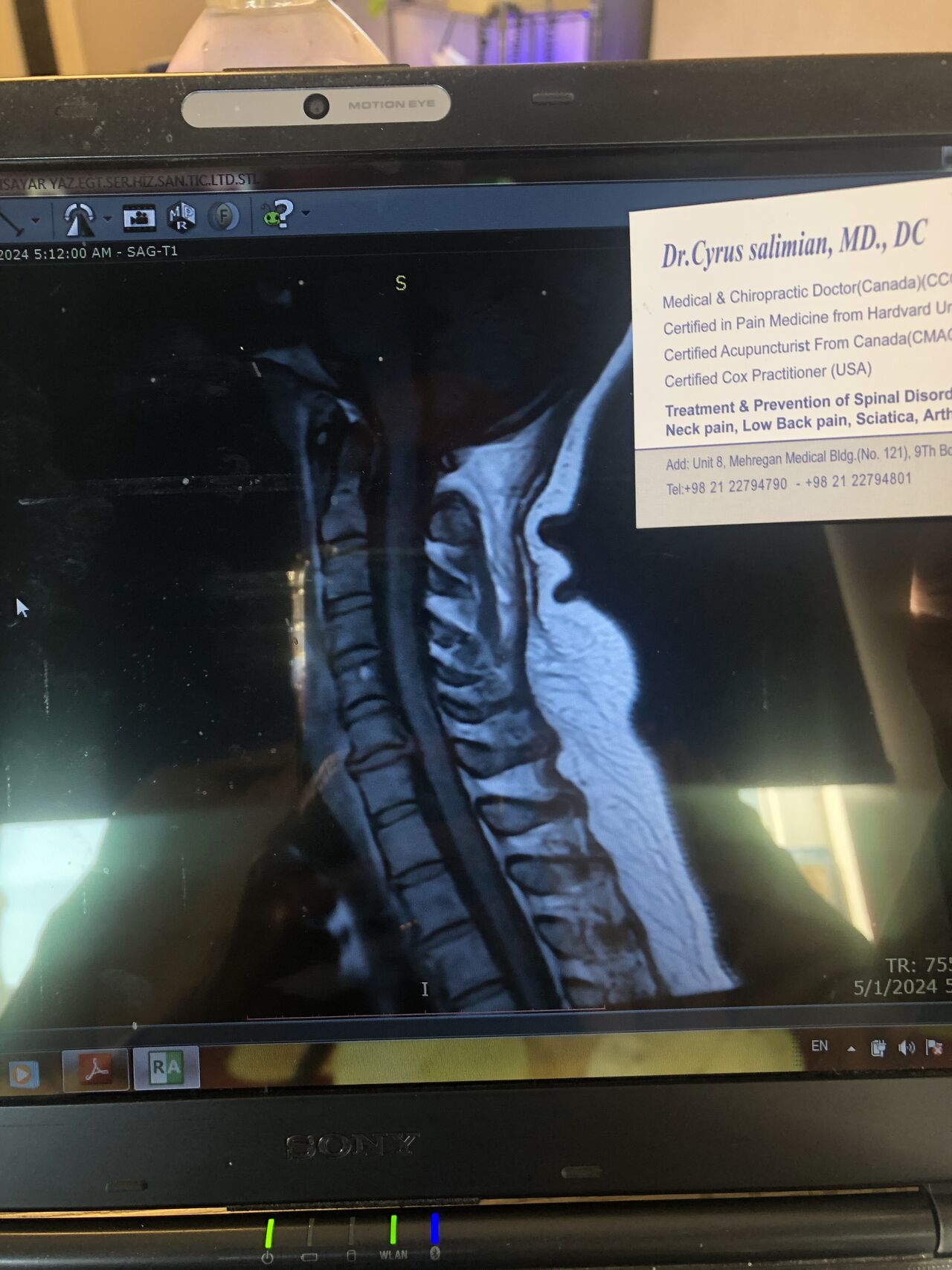
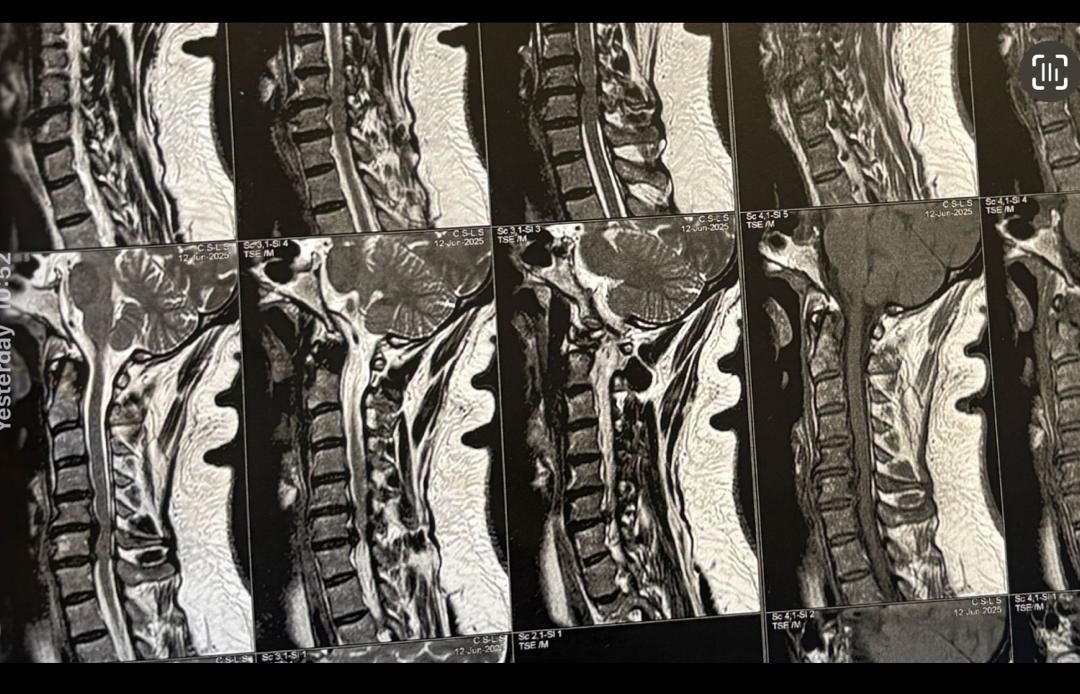
30 year old patient of mine with R. IVF disc extrusion of C 5-6 with R upper extremity pain and numbness without neurological deficit was suggested to have urgent surgery
in his EMG. NCV didn’t have any active axonal loss
got 20 sessions of chiropractic care in one month by me mainly using decompression and C0-C1 prone drop manipulation and 3 sessions of mild adjustment to segments above disc herniation. No direct adjustment to the involved disc extrusion
After treatment:
reduction of R. IVFdisc extrusion by more than 50%.
90% improvement in patient’s signs and symptoms and preventing of unnecessary expensive surgery
following one month of cervical chiropractic spinal treatments
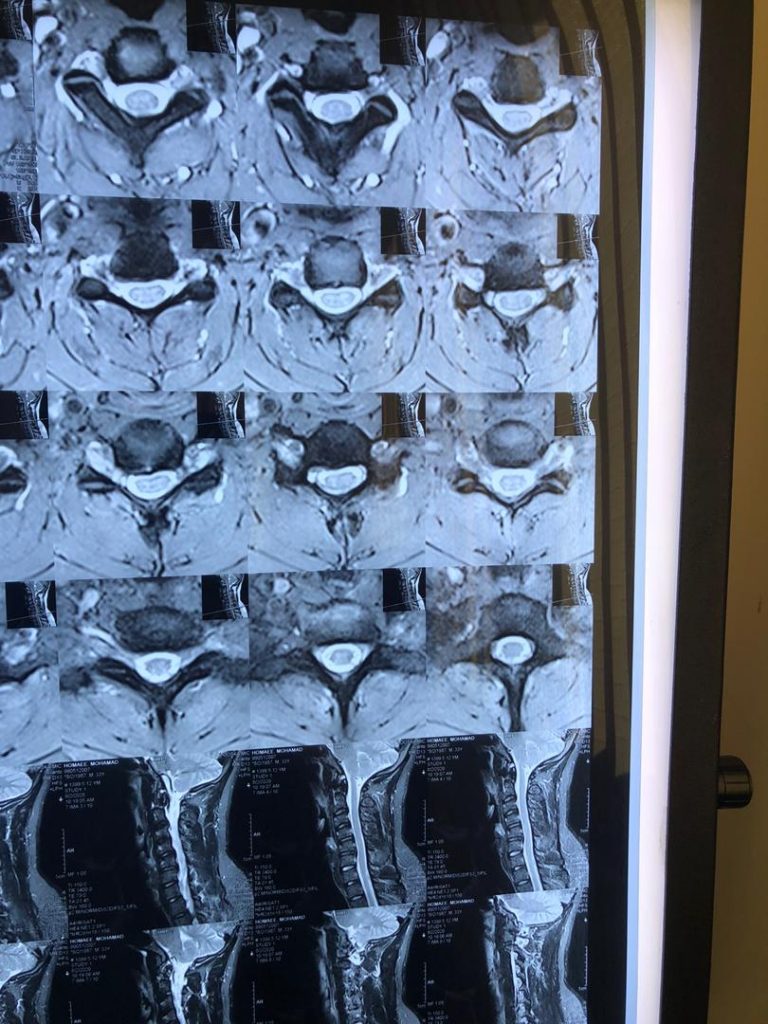
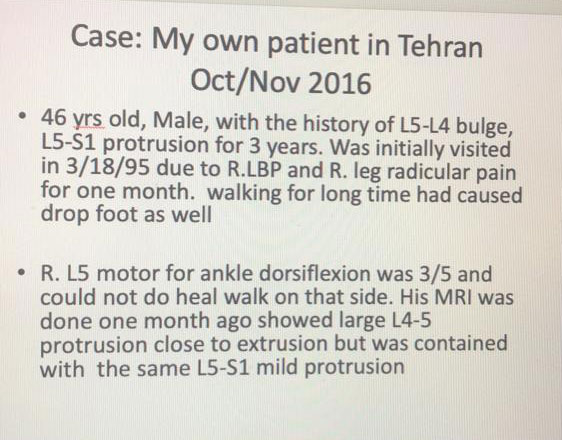
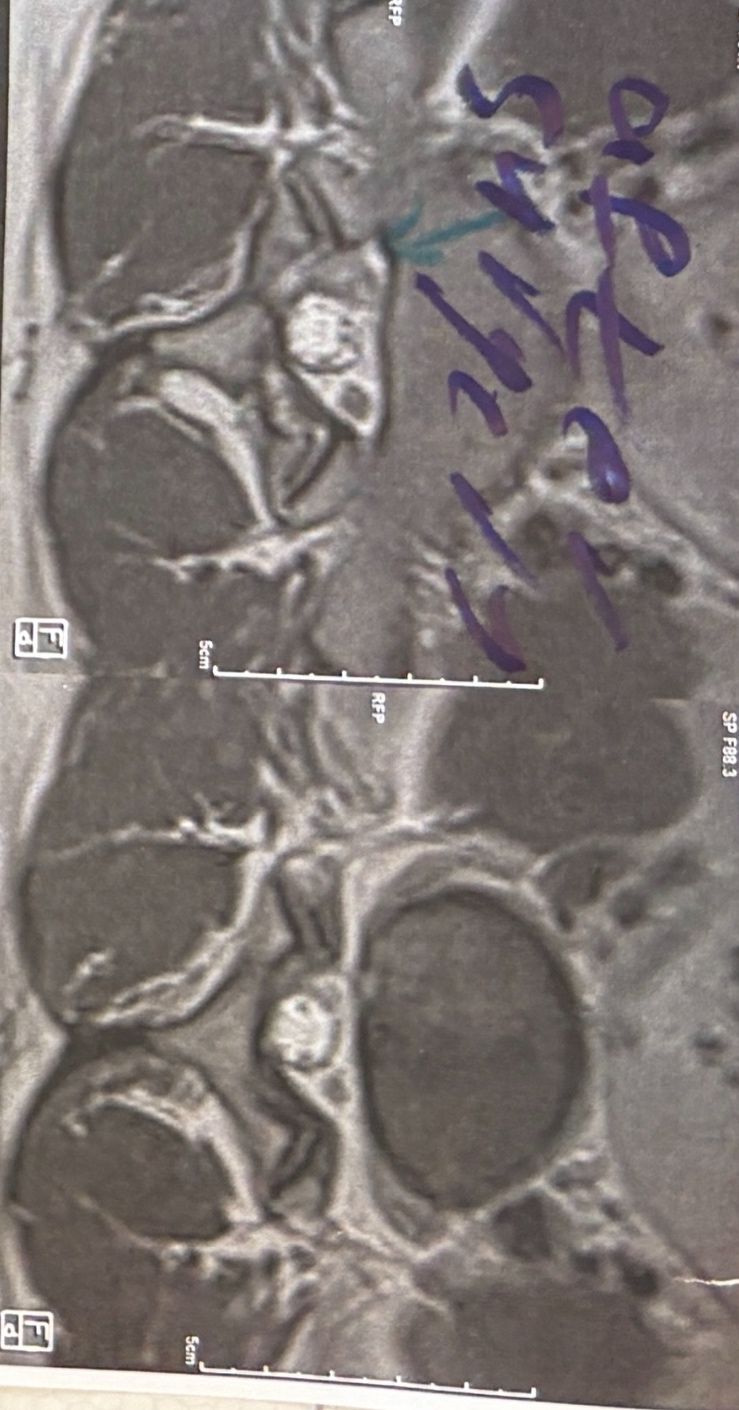
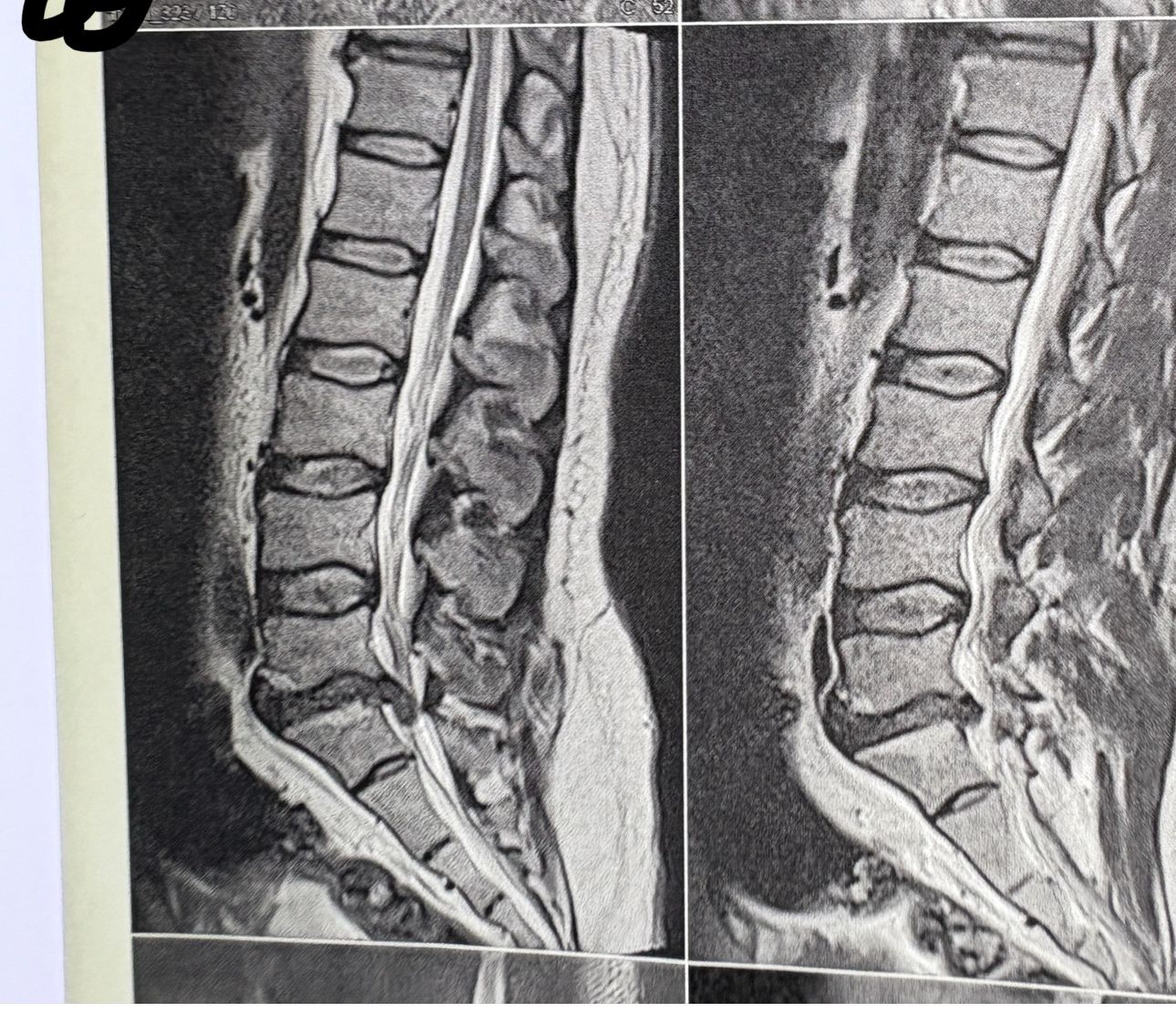
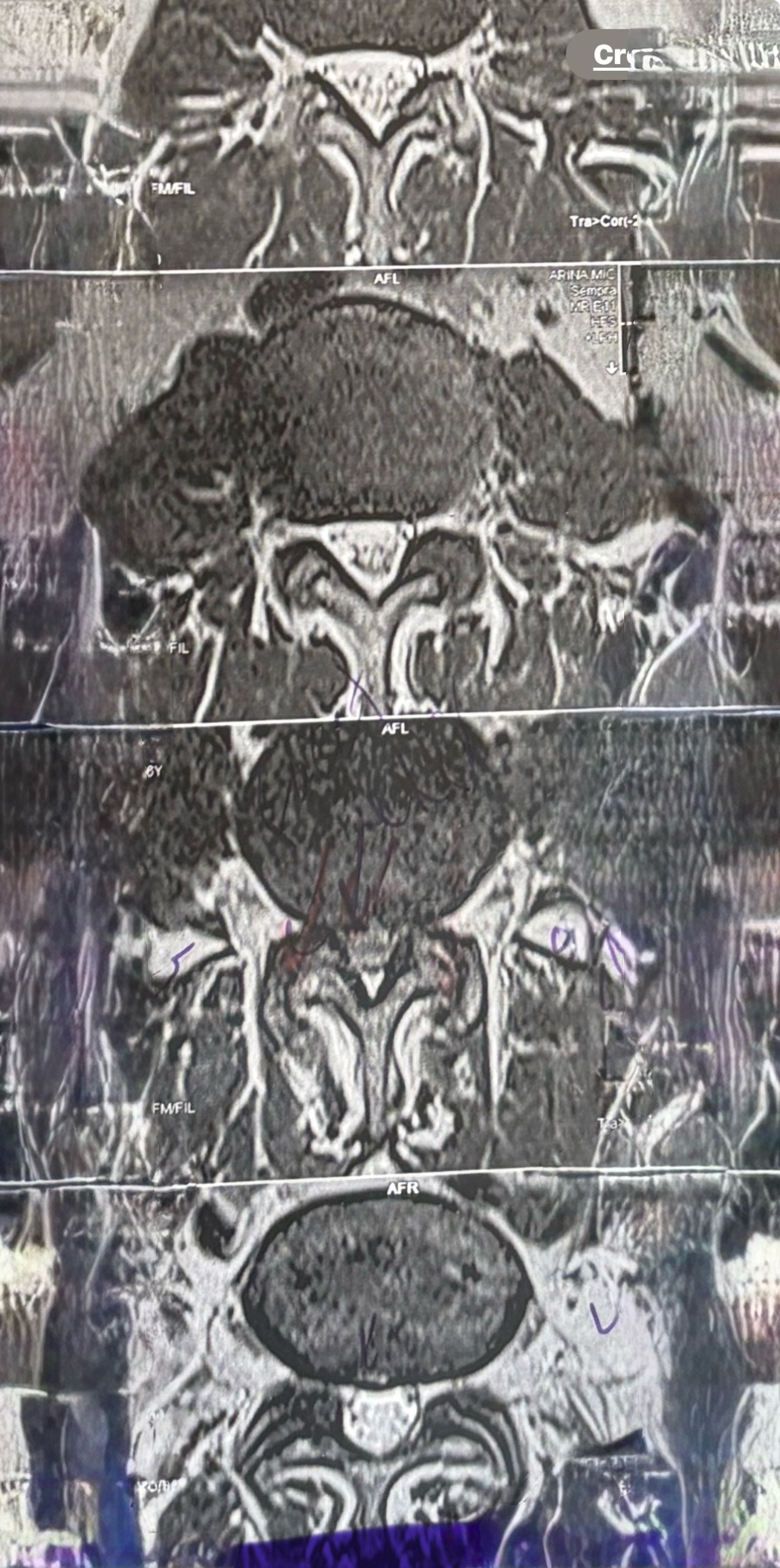
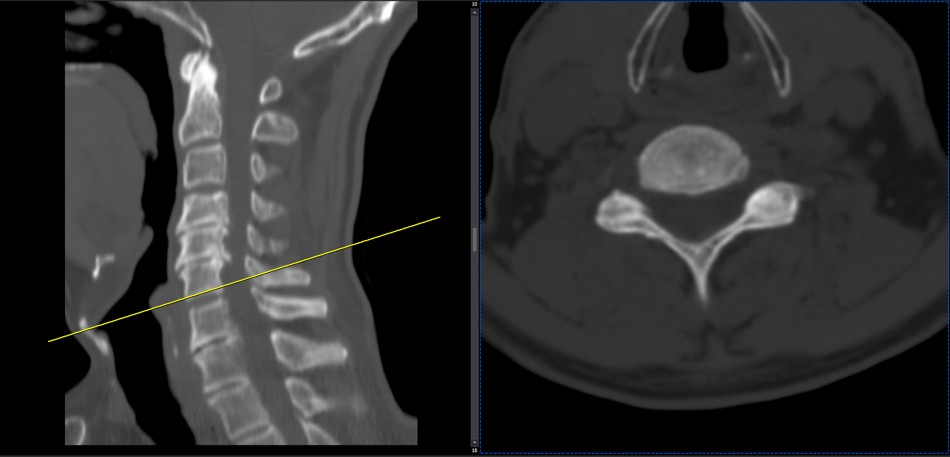
Case 2
After 28 sessions of spinal chiropractic treatments by me using Decompression techniques. without using chiropractic adjustment to the involved disc which is contraindicated in disc extrusions
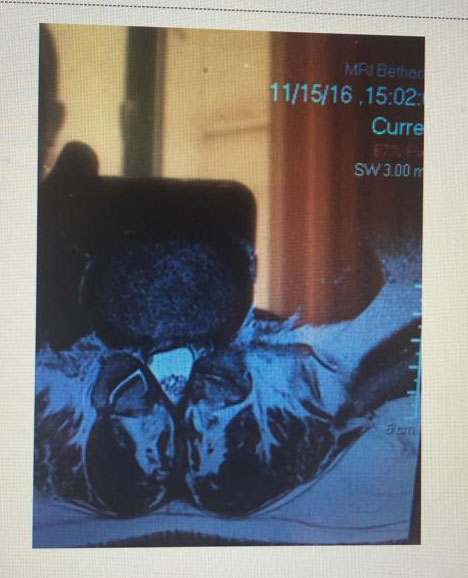
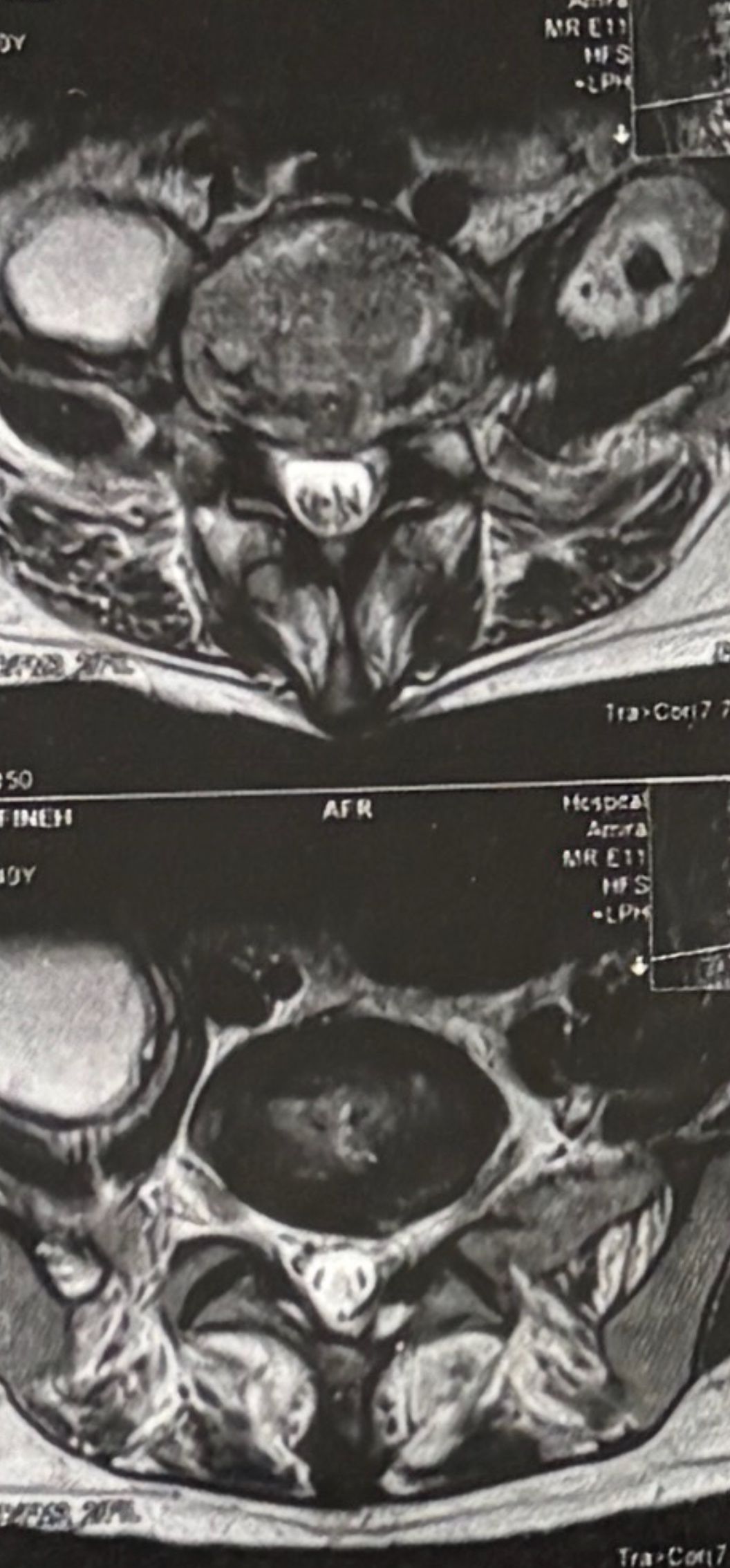
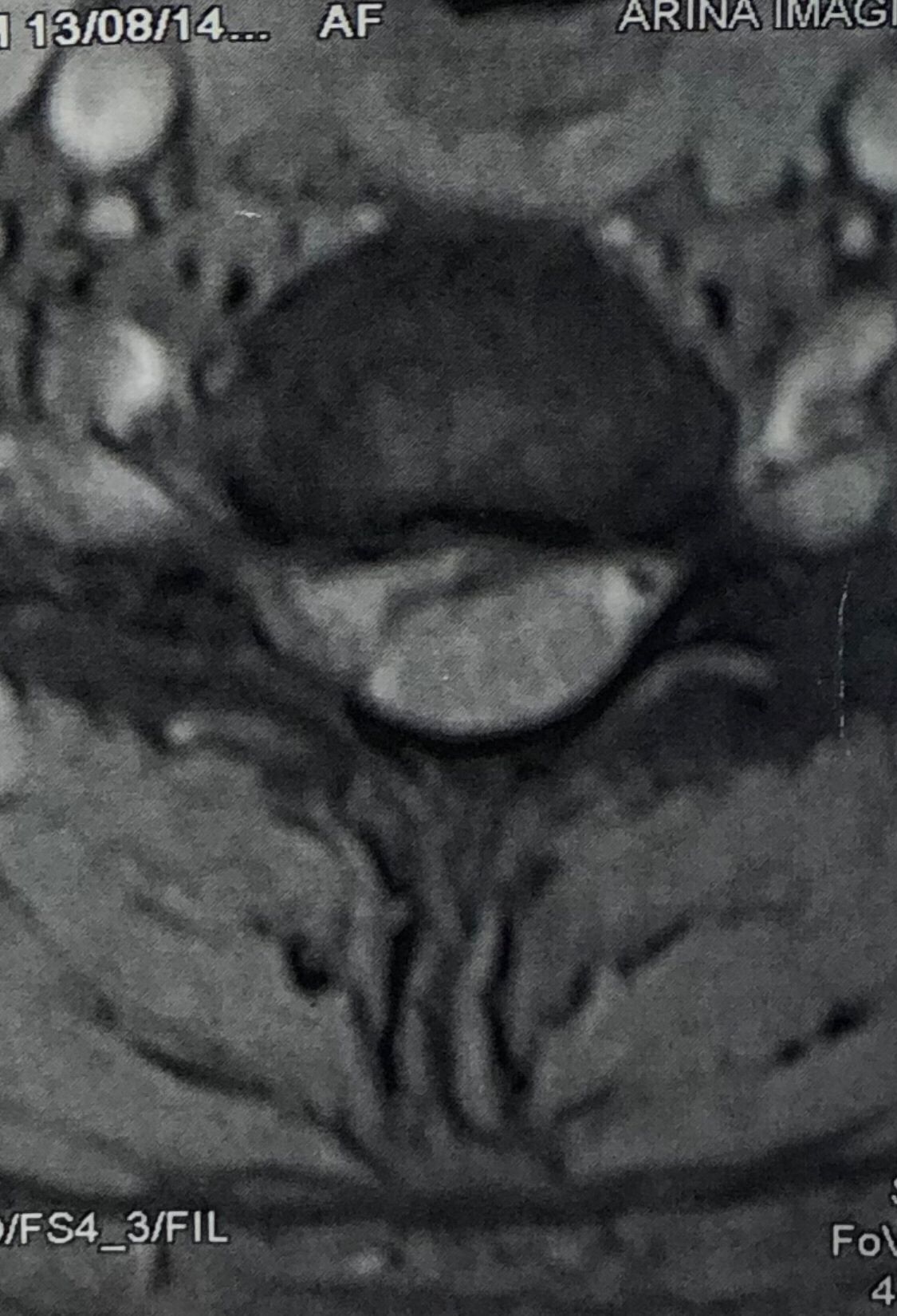
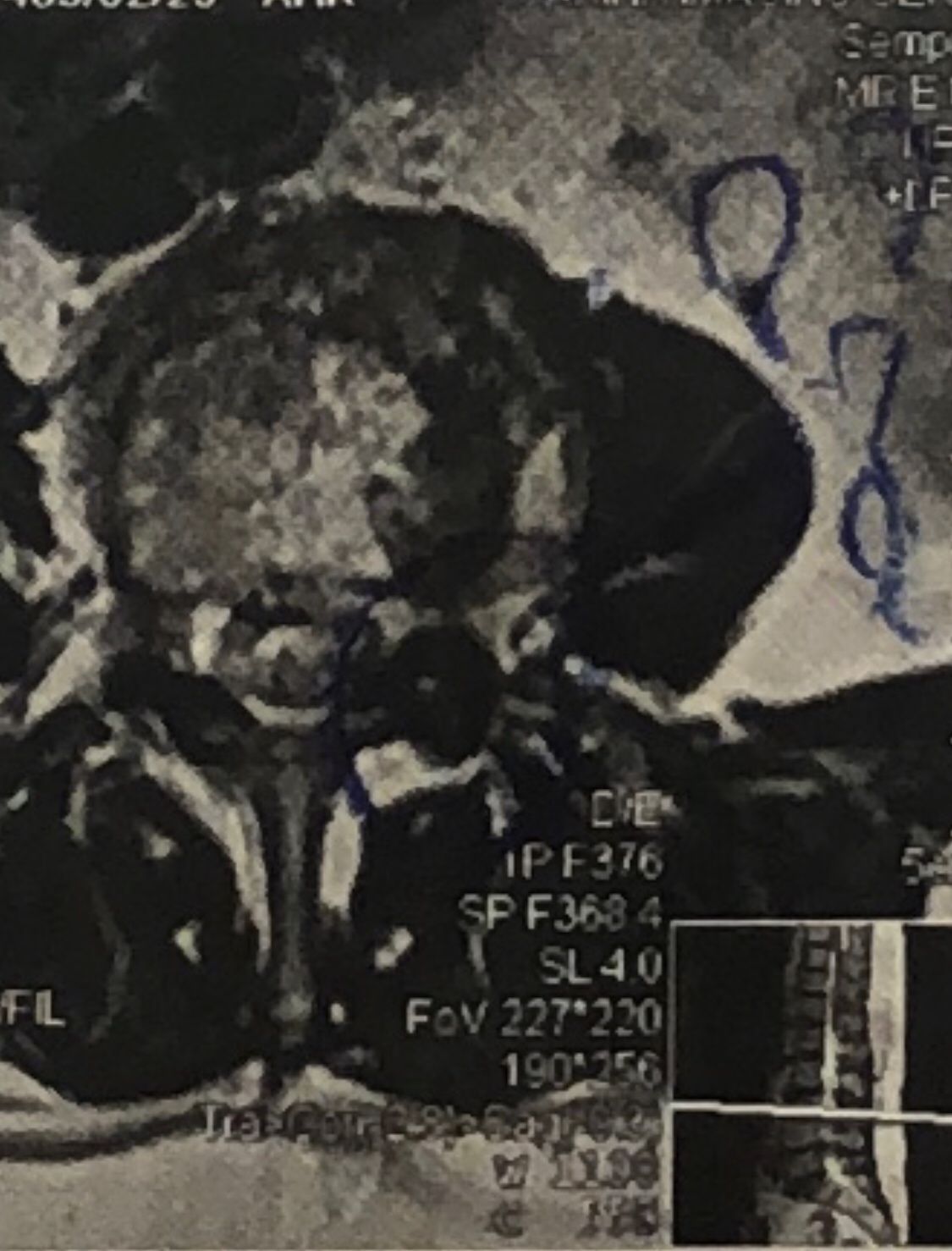
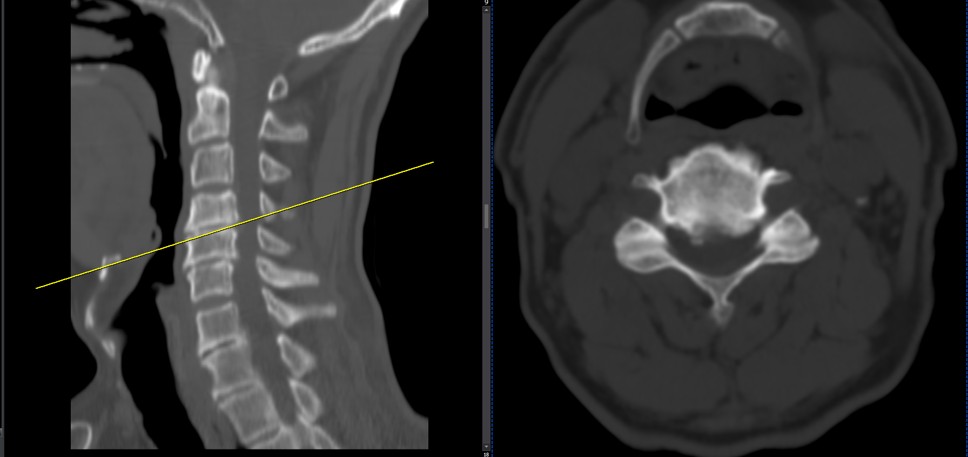
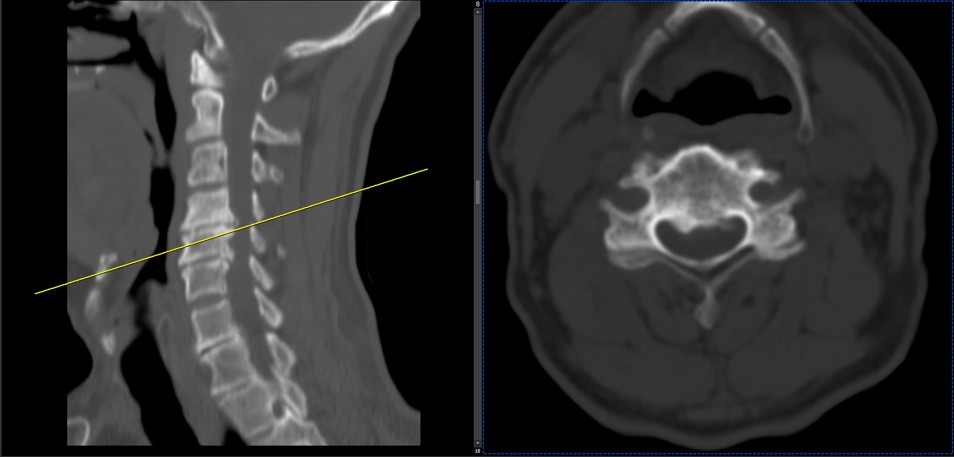
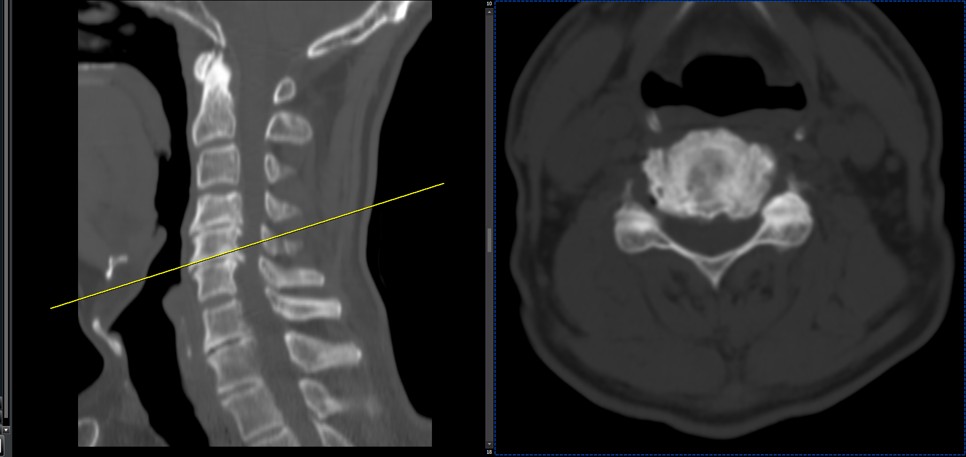
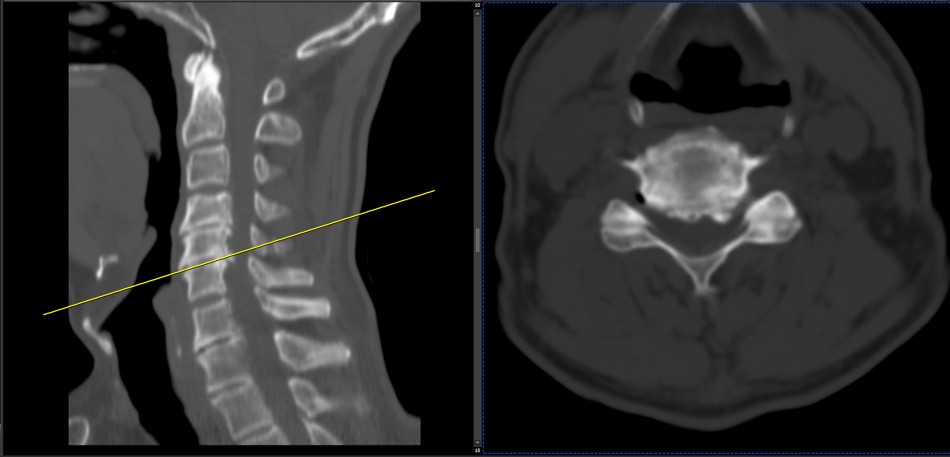
Case 4
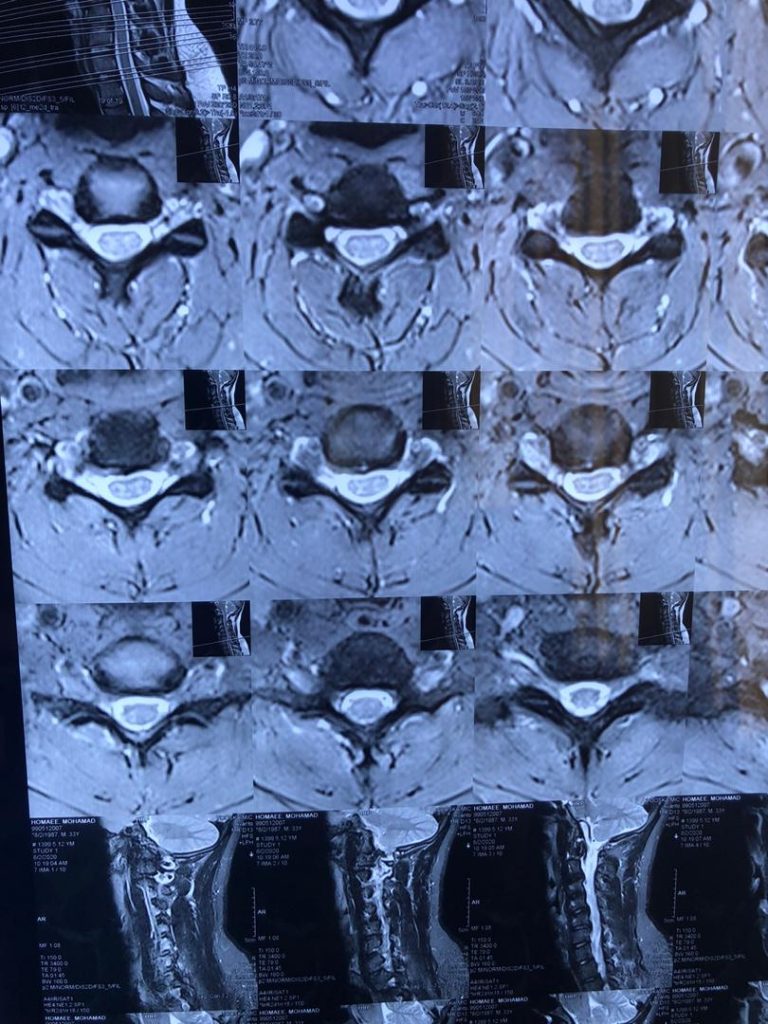
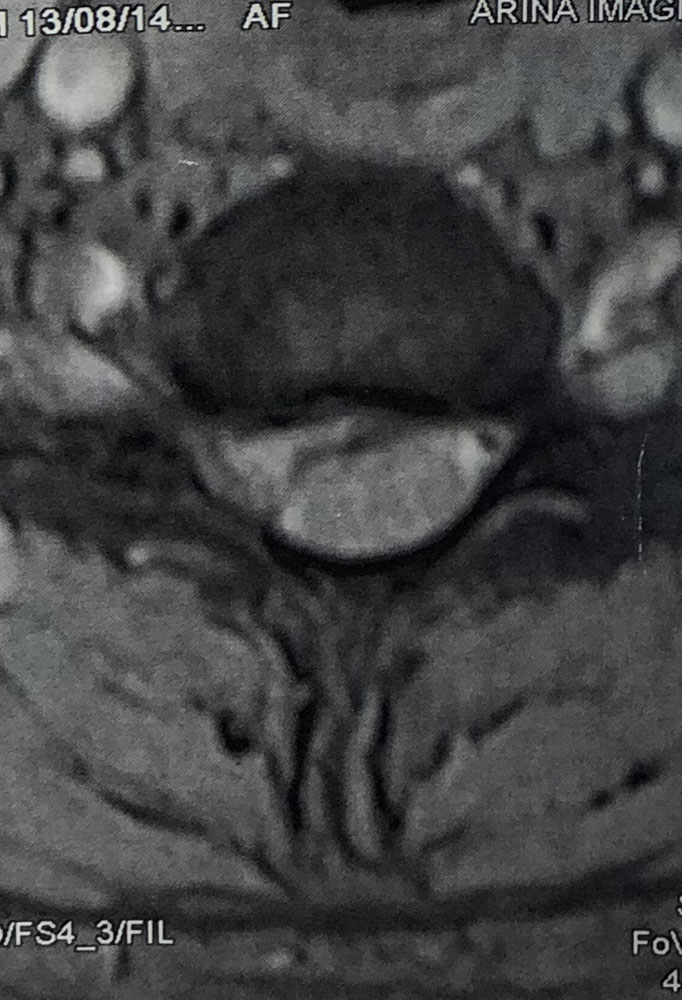
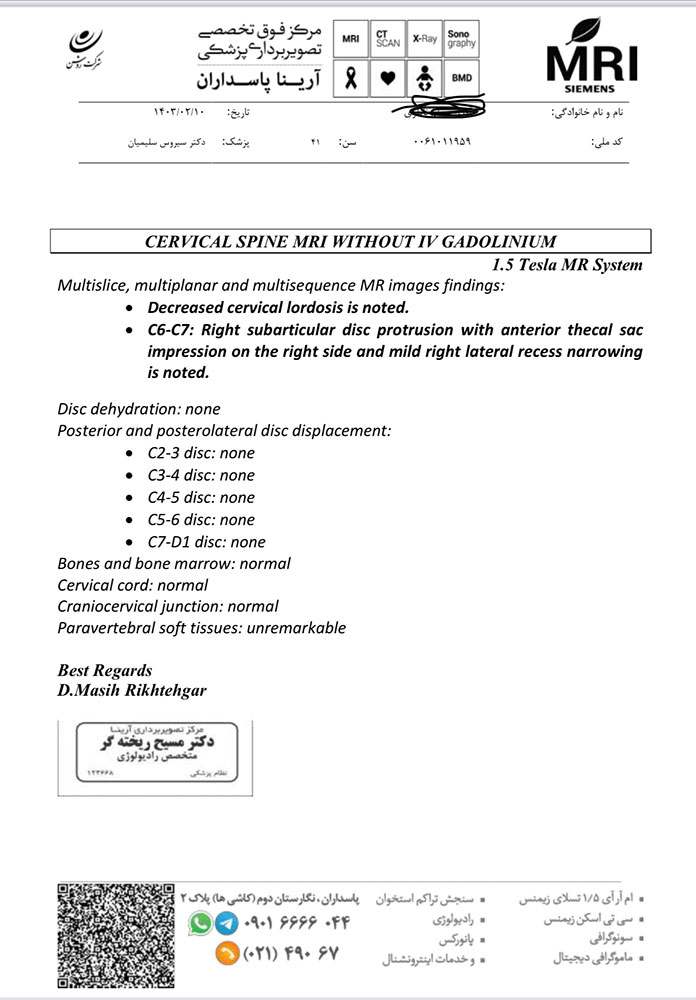
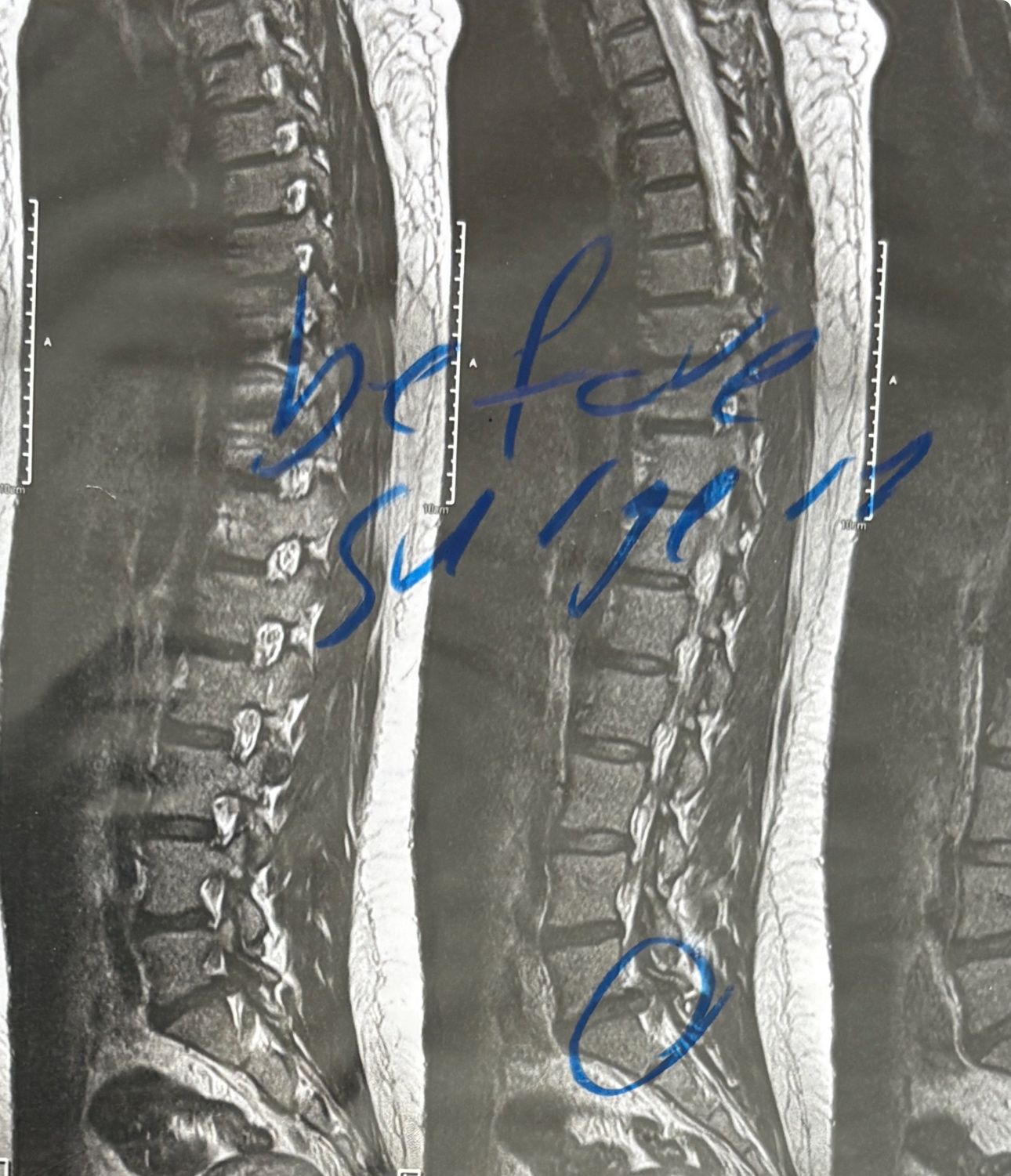
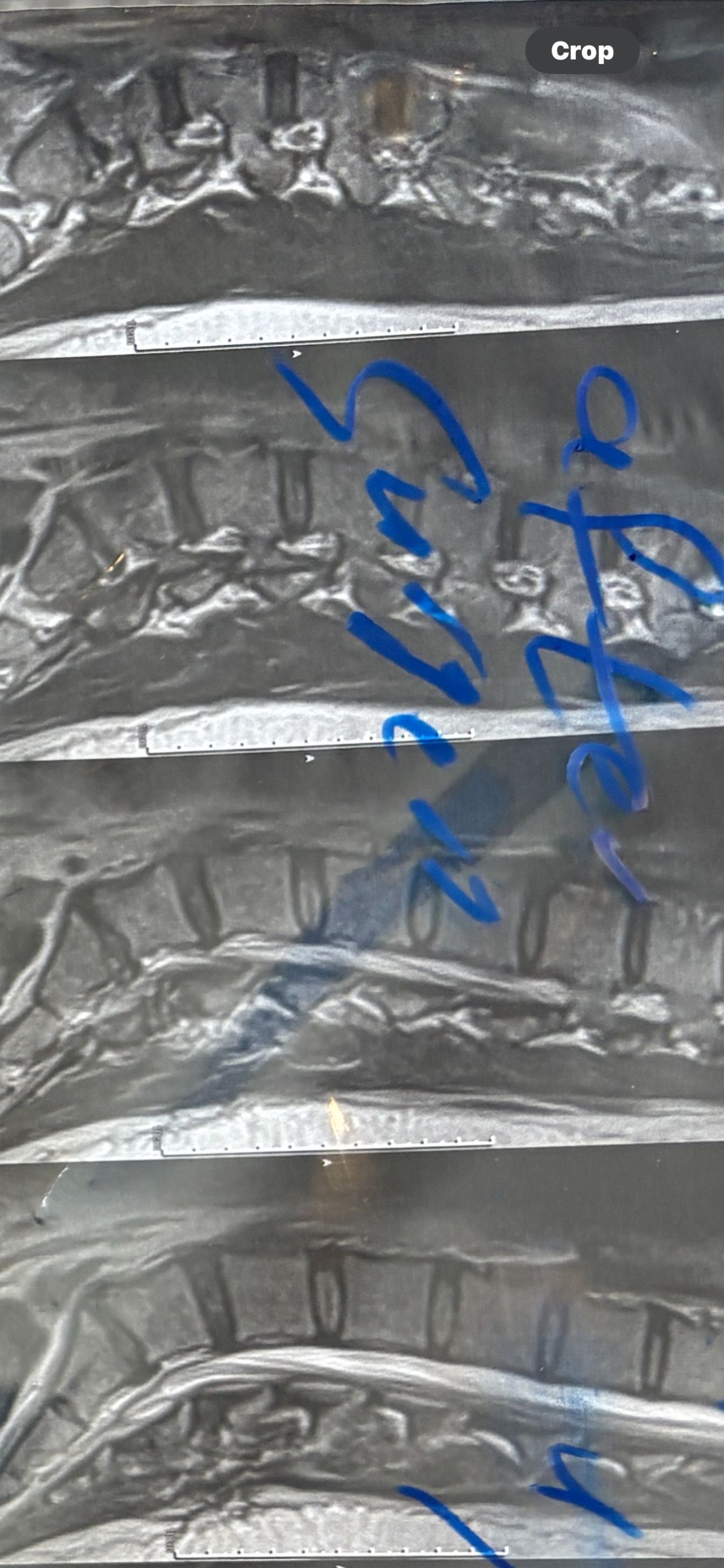
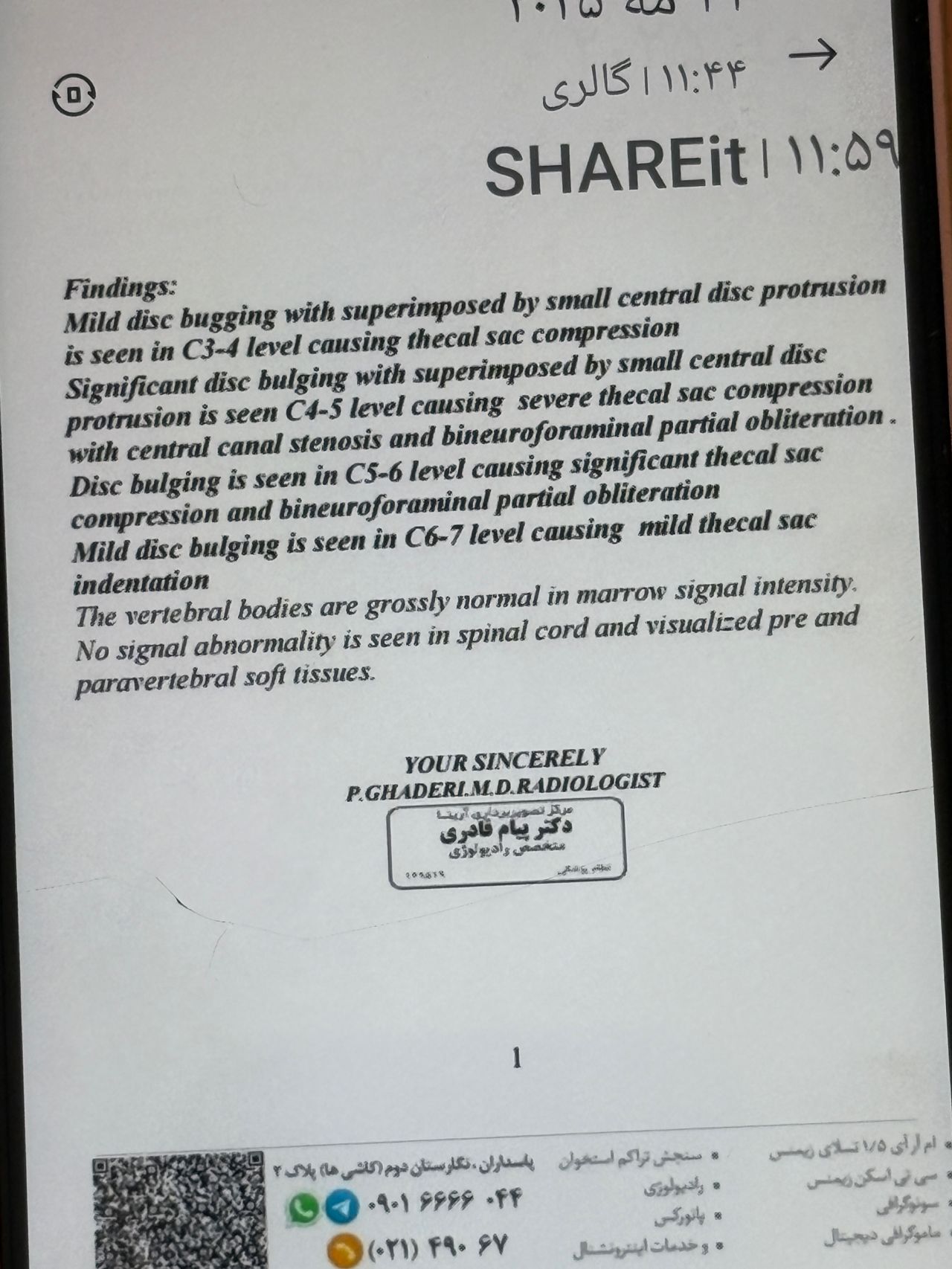
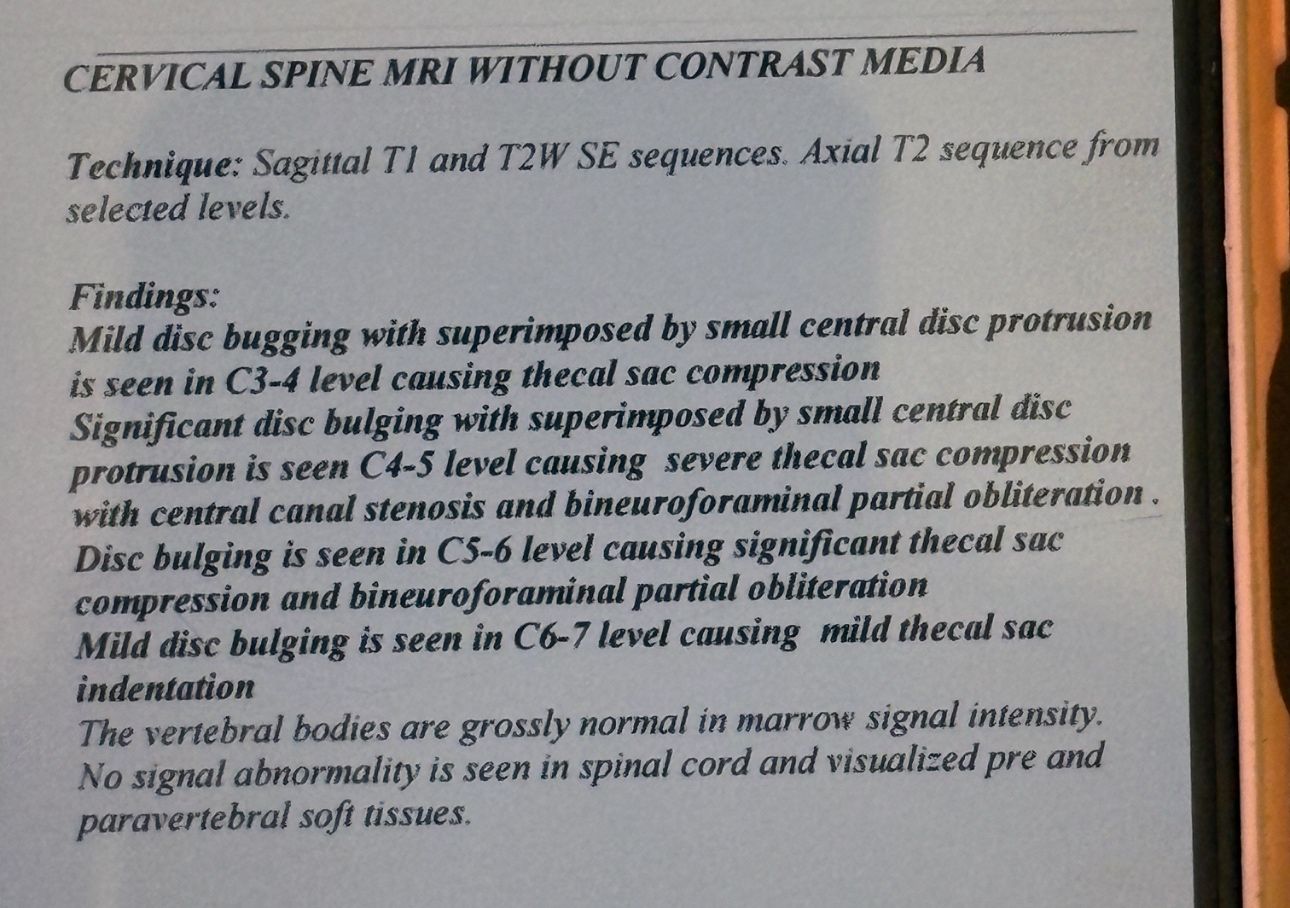
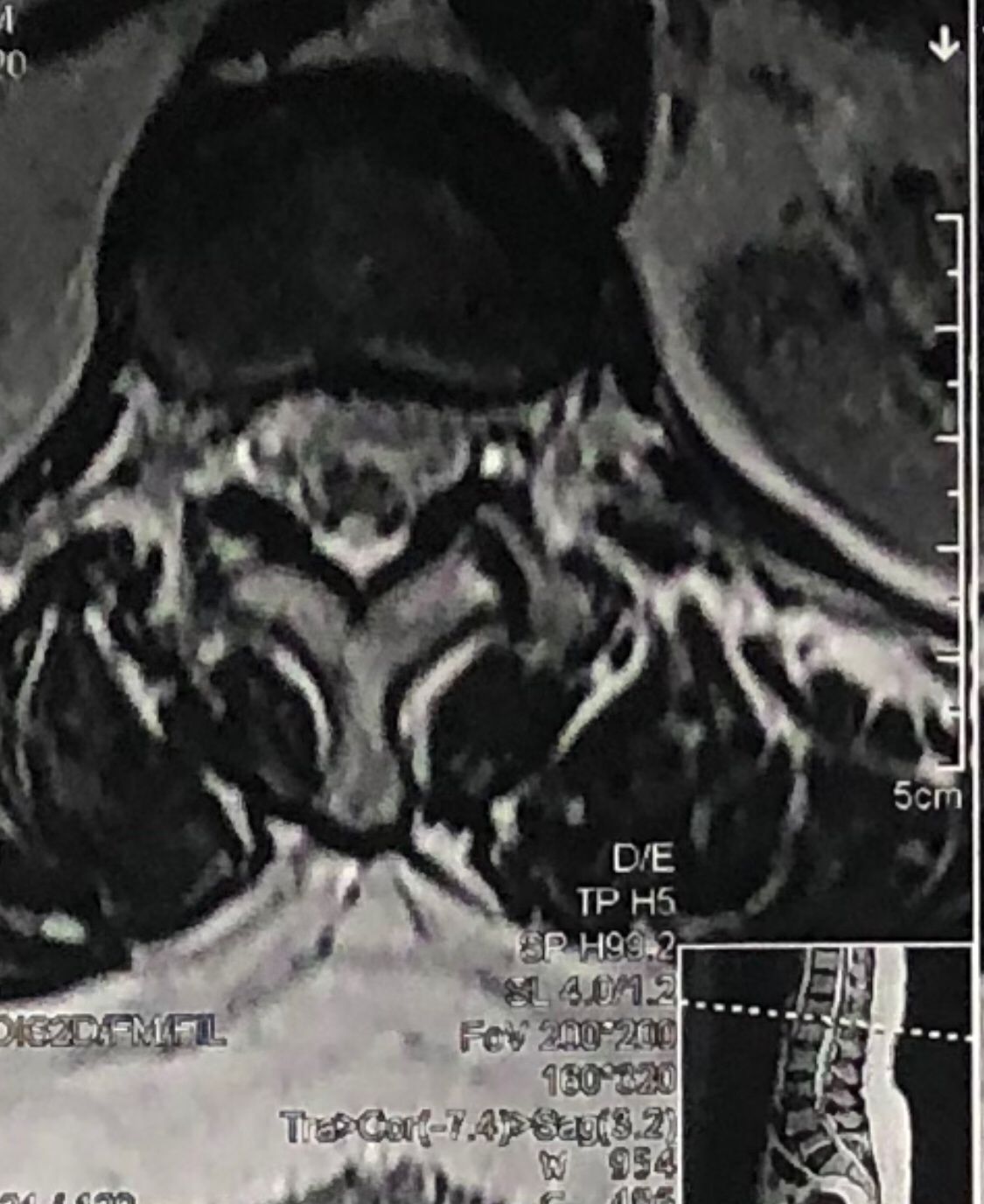
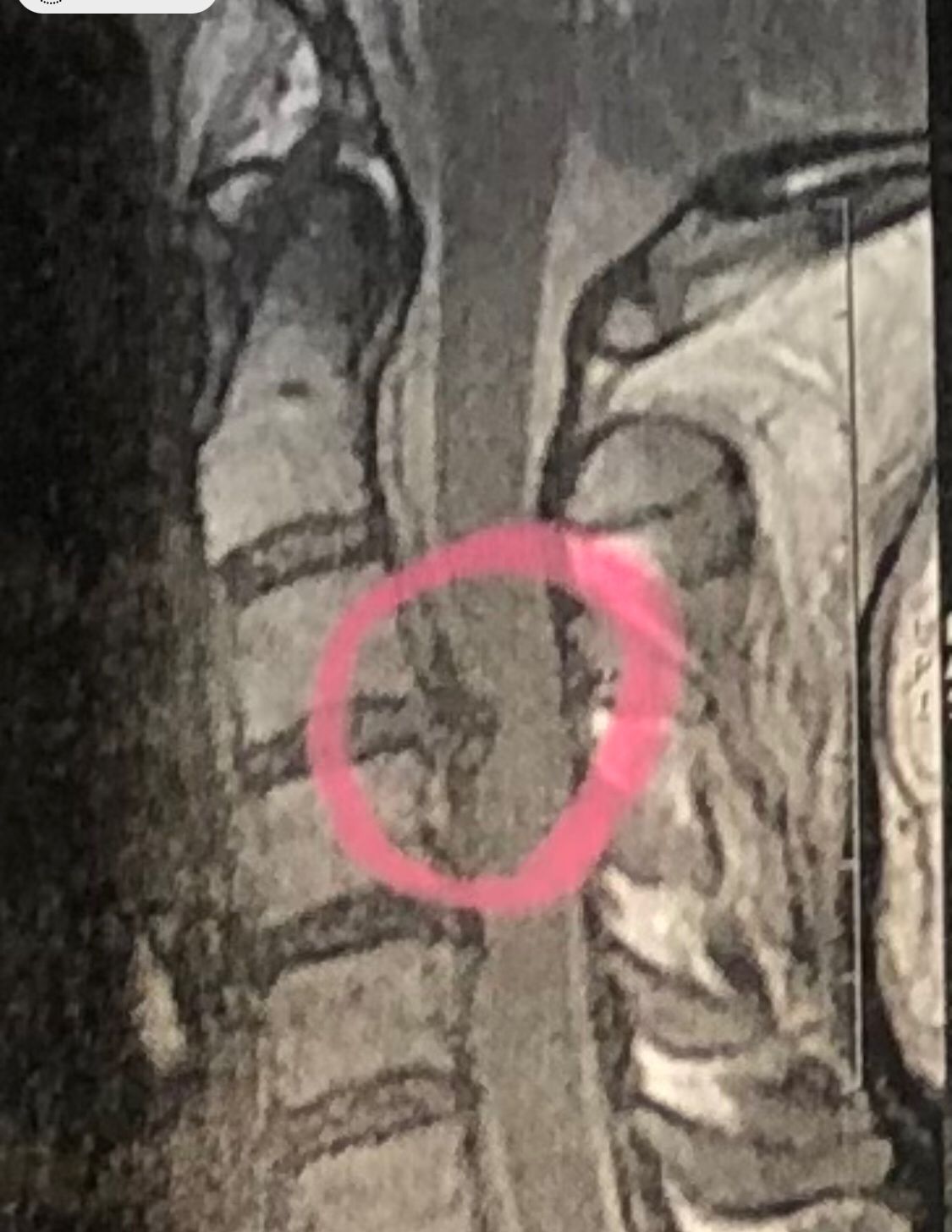
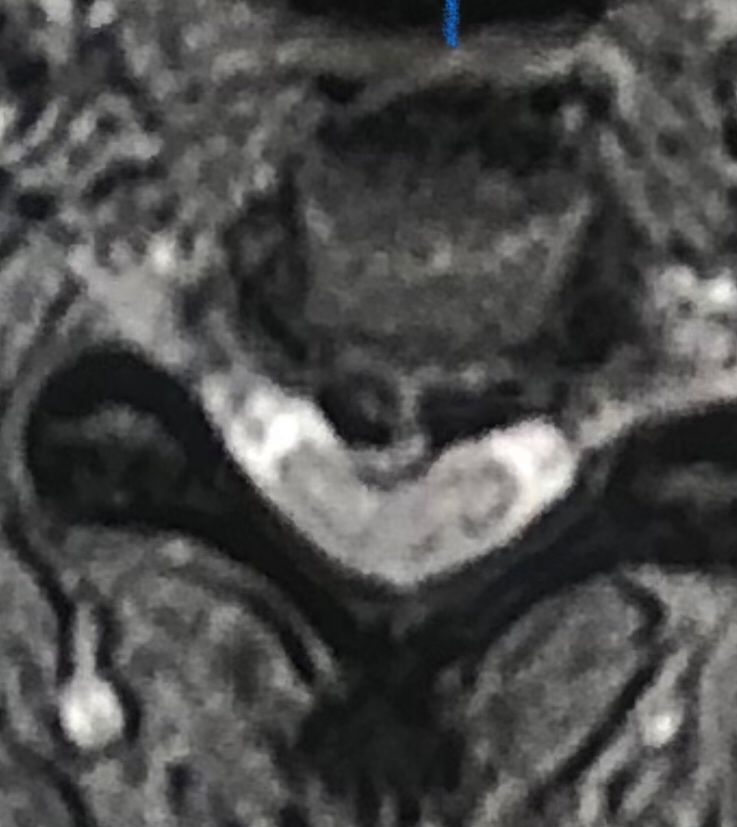
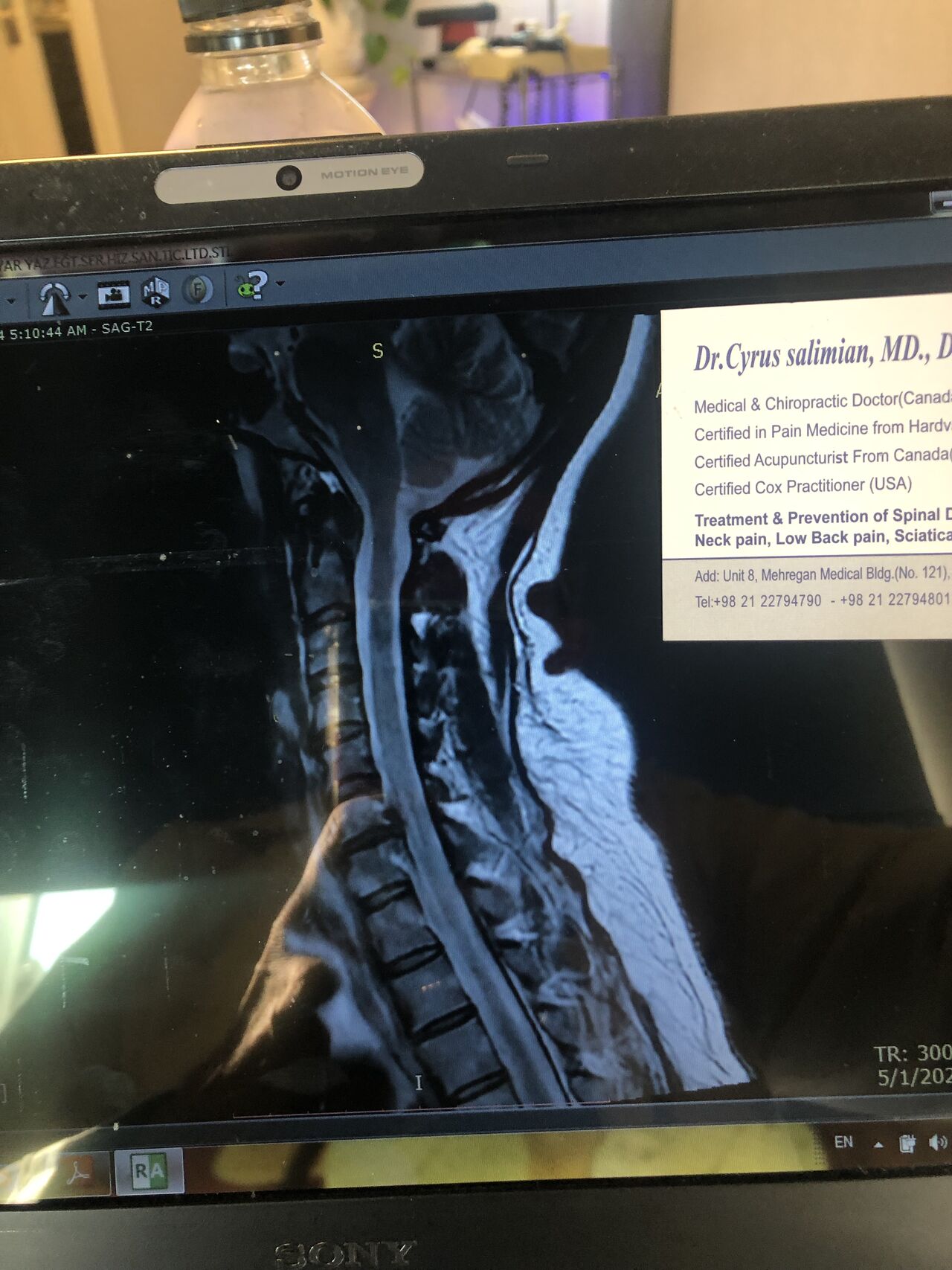
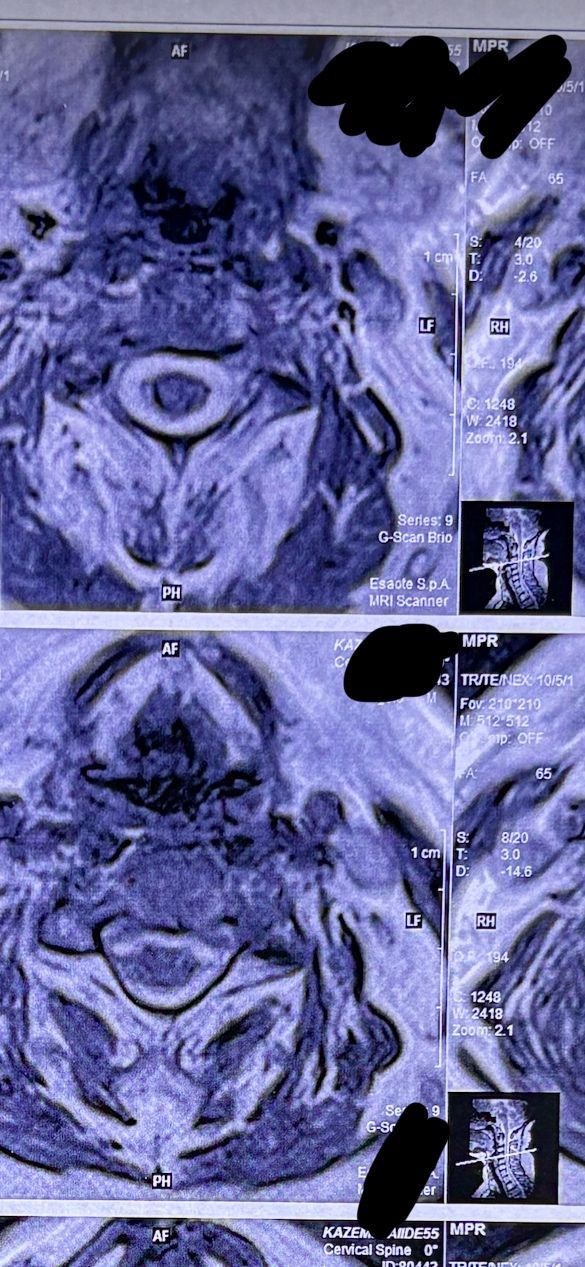
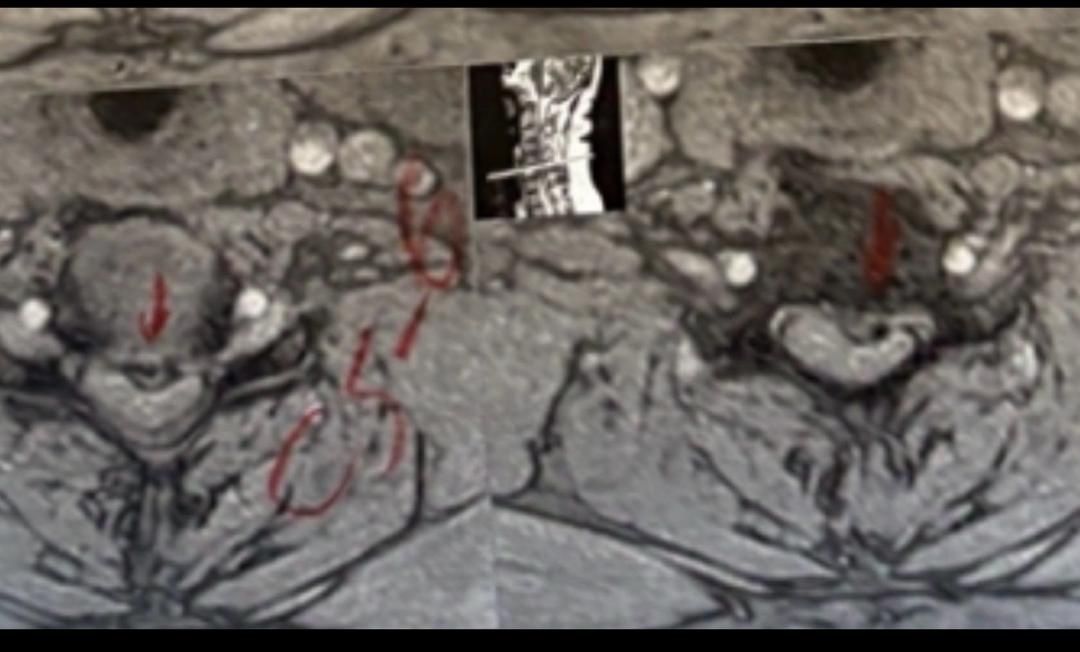
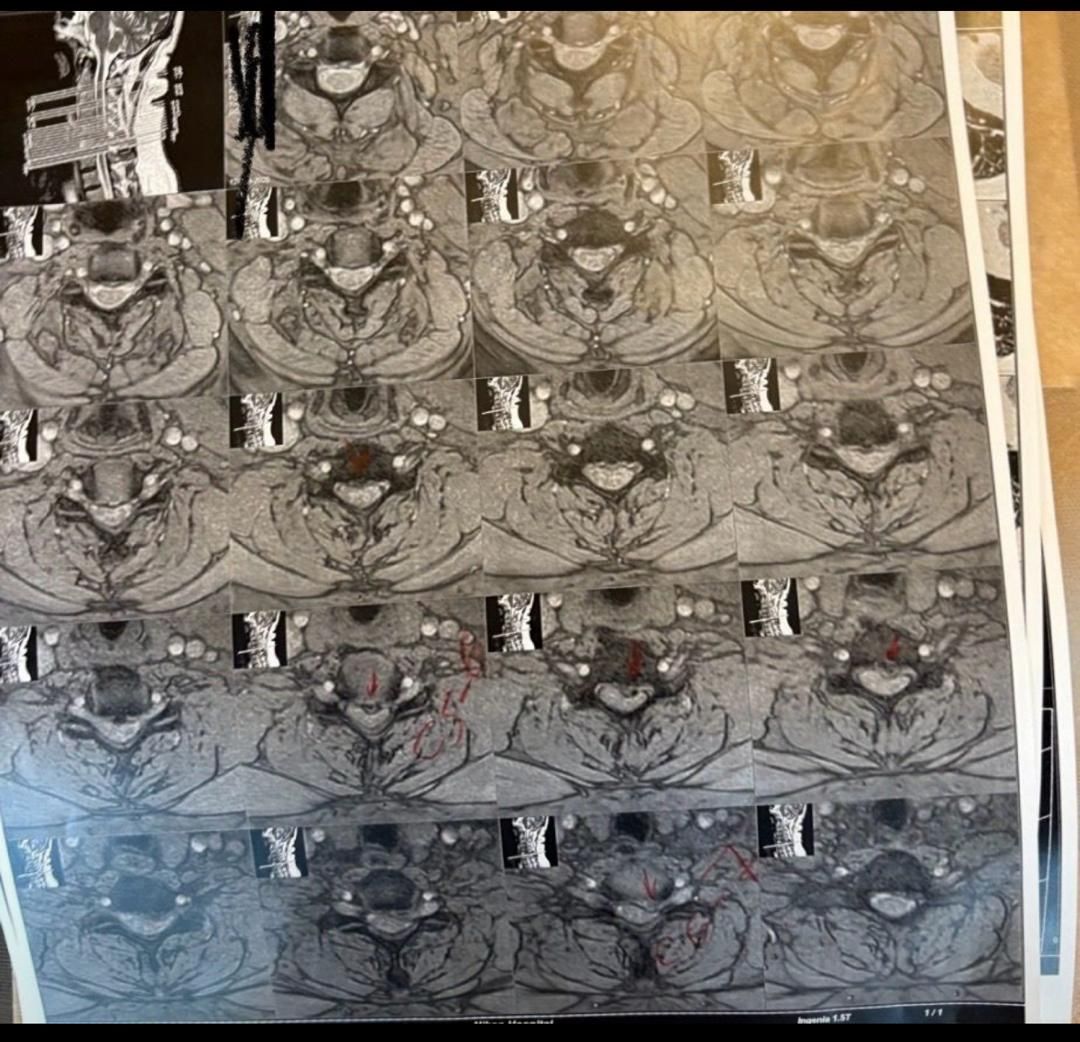
41 years old man presented to my clinic in October 2023 with acute and sever R neck pain with radicular pain to his R upper extremity along C6 dematom since 2 weeks ago. Examination didn’t show any upper motor signs. Was suggested urgent surgery
I ordered EMG/ NCV : showed mild R C6, C7 irritation without any active axonal loss
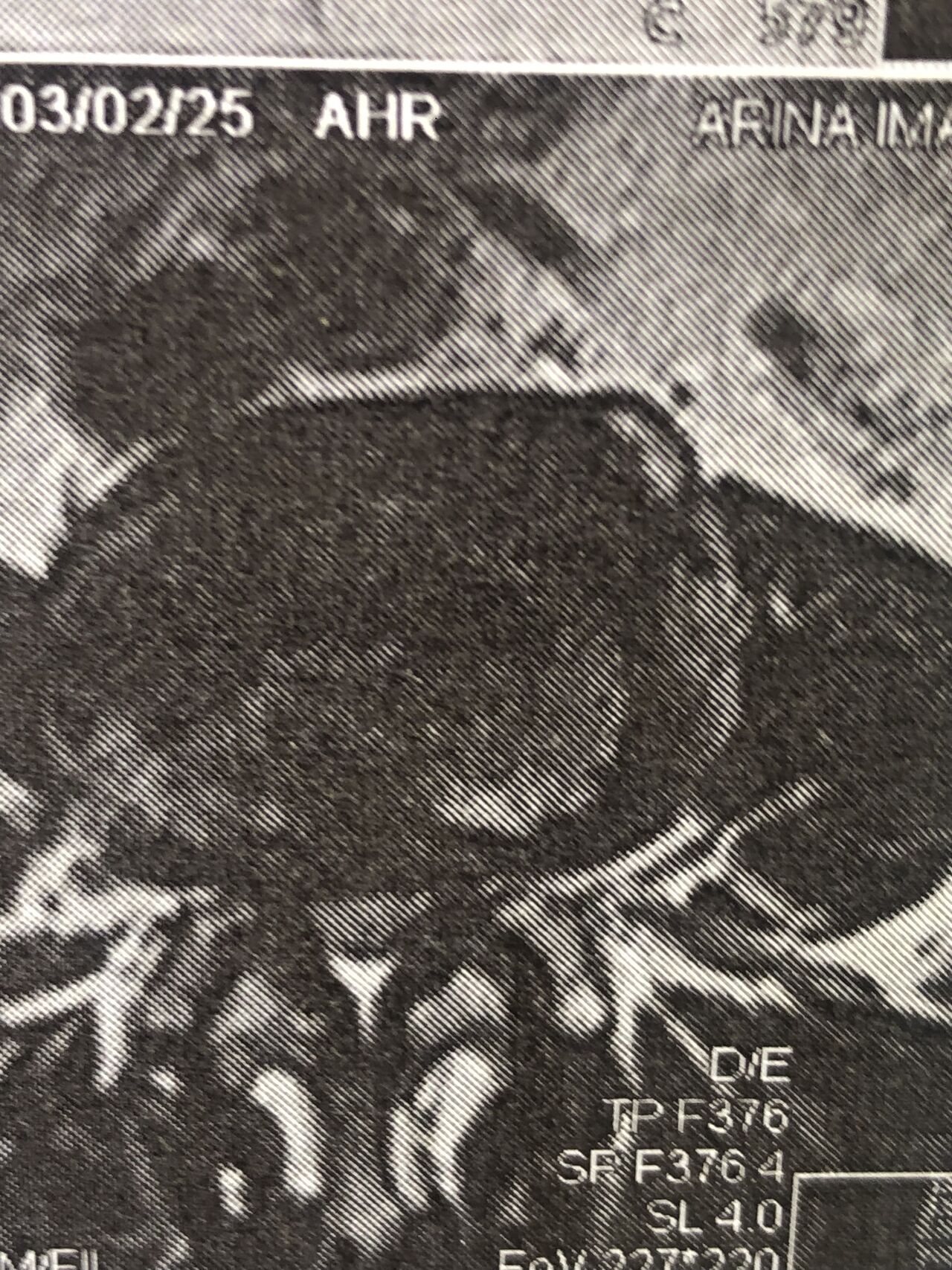
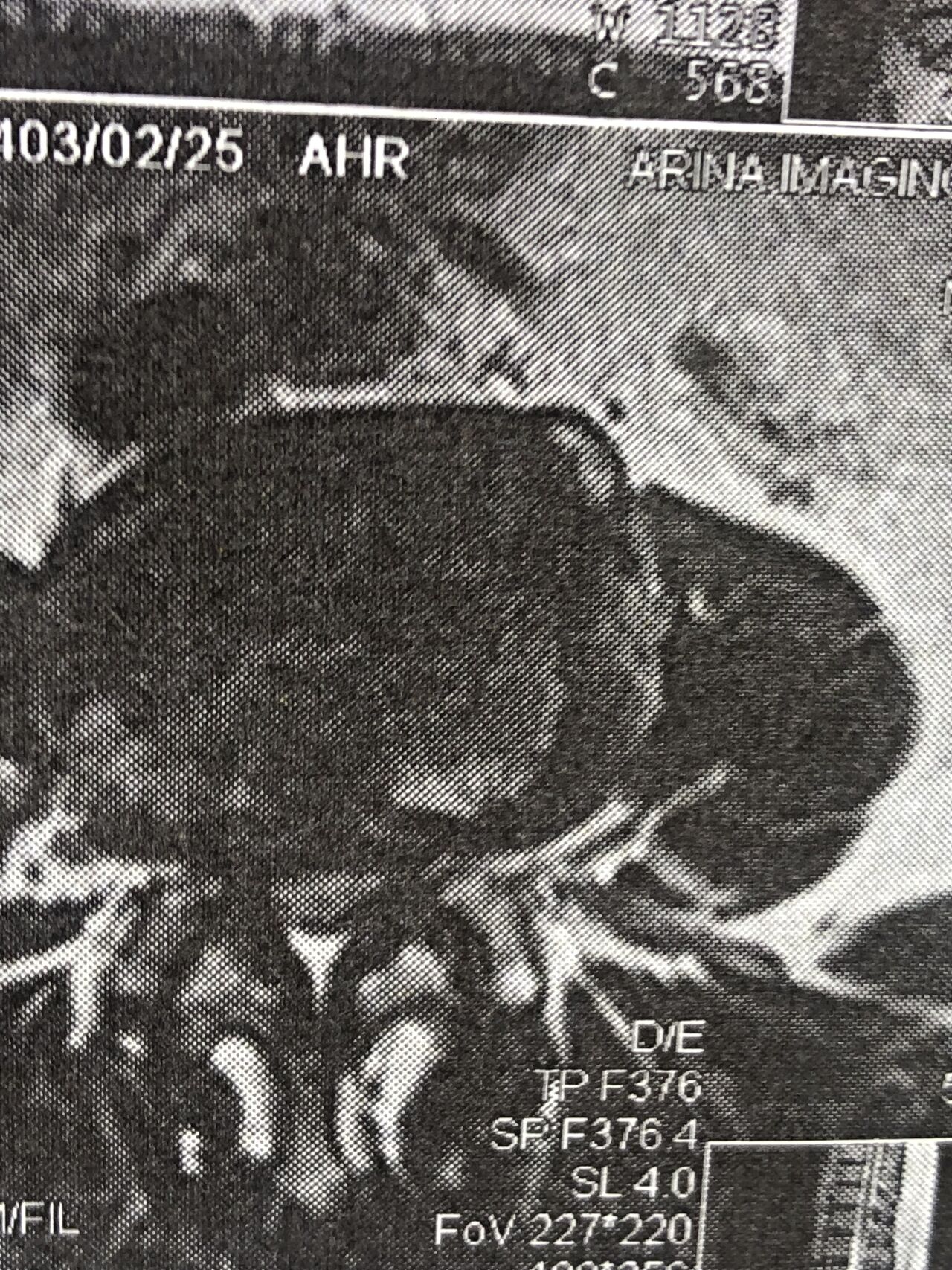
In his MRI was reported R. para R. IVF Massive extrusion. I decided to control his pain and manage this patient with reevaluation of patient every other session. For 5 sessions i just used acupuncture and laser and IFC and mild adjustments to his R. T3-T7 and mild arthosteem to above and below involved segment. Cervical adjustment considered contraindicated for this patient. From session 6th- 8th i started to use mild/gentle cervical decompression. He used soft cervical collar all the time. His pain decreased by 80 percent
I gave him cervical traction pump to be used 3-5 times per day at home for the next 3 months and i released the patient. He was evaluated every week once for one month and after that every 2 weeks. After 3 month I repeated MRI. Size of the herniated disc was reduced greater than 50 percent. Asked him to do another mri in 6 months
In general: Precise selection of the patients, examination,diagnosis, plan of management, reevaluation and treatment can be done by doctors of chiropractic for the patients with spinal disc herniation and stenosis Moreover giving reasonable time to these kind of patients under direct supervision by their chiropractic doctors can prevent unnecessary surgery. Proper selection of these kind of patients is another important fact that can be done precisely by chiropractors.
MRIs before and after proper management of this patient:
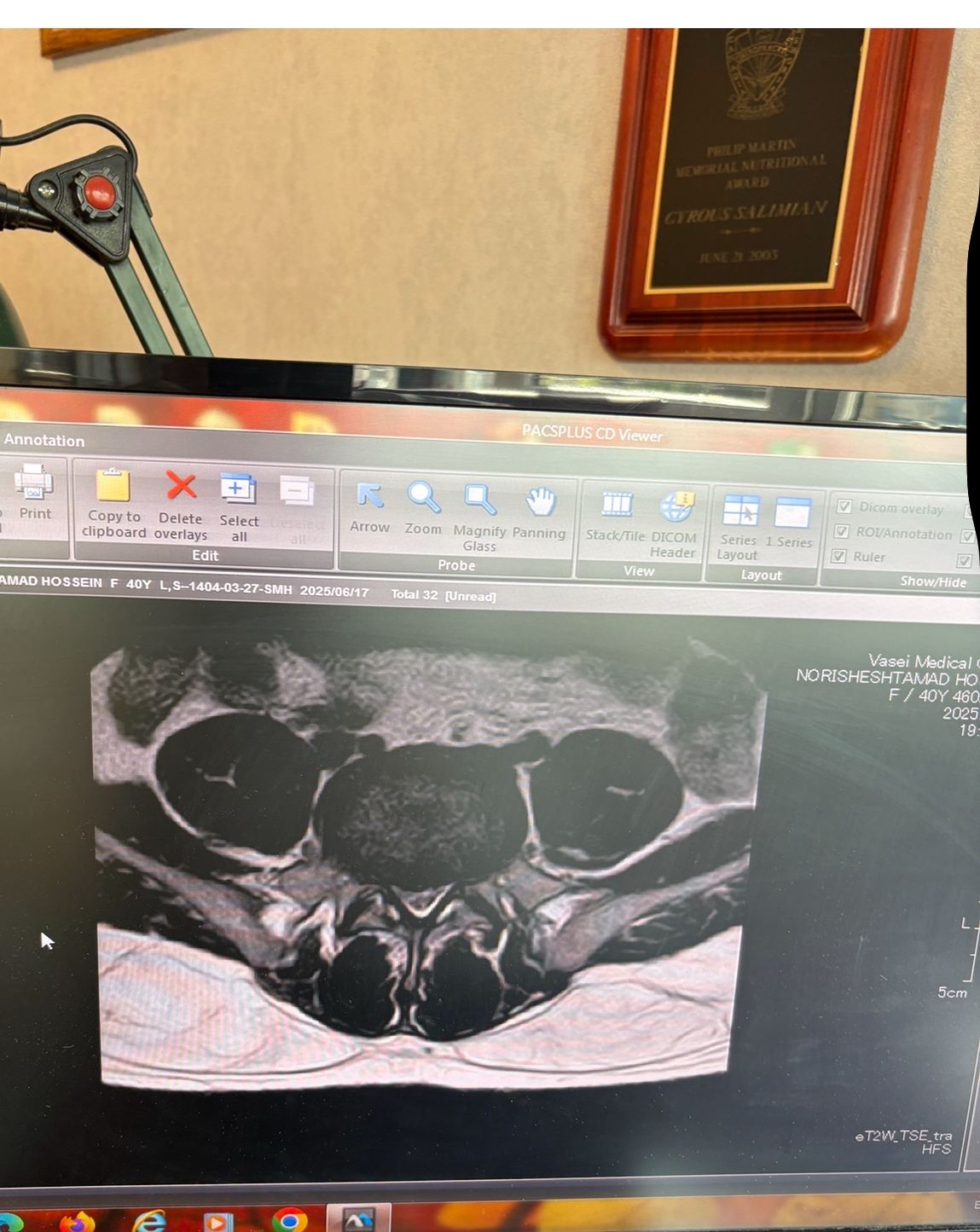
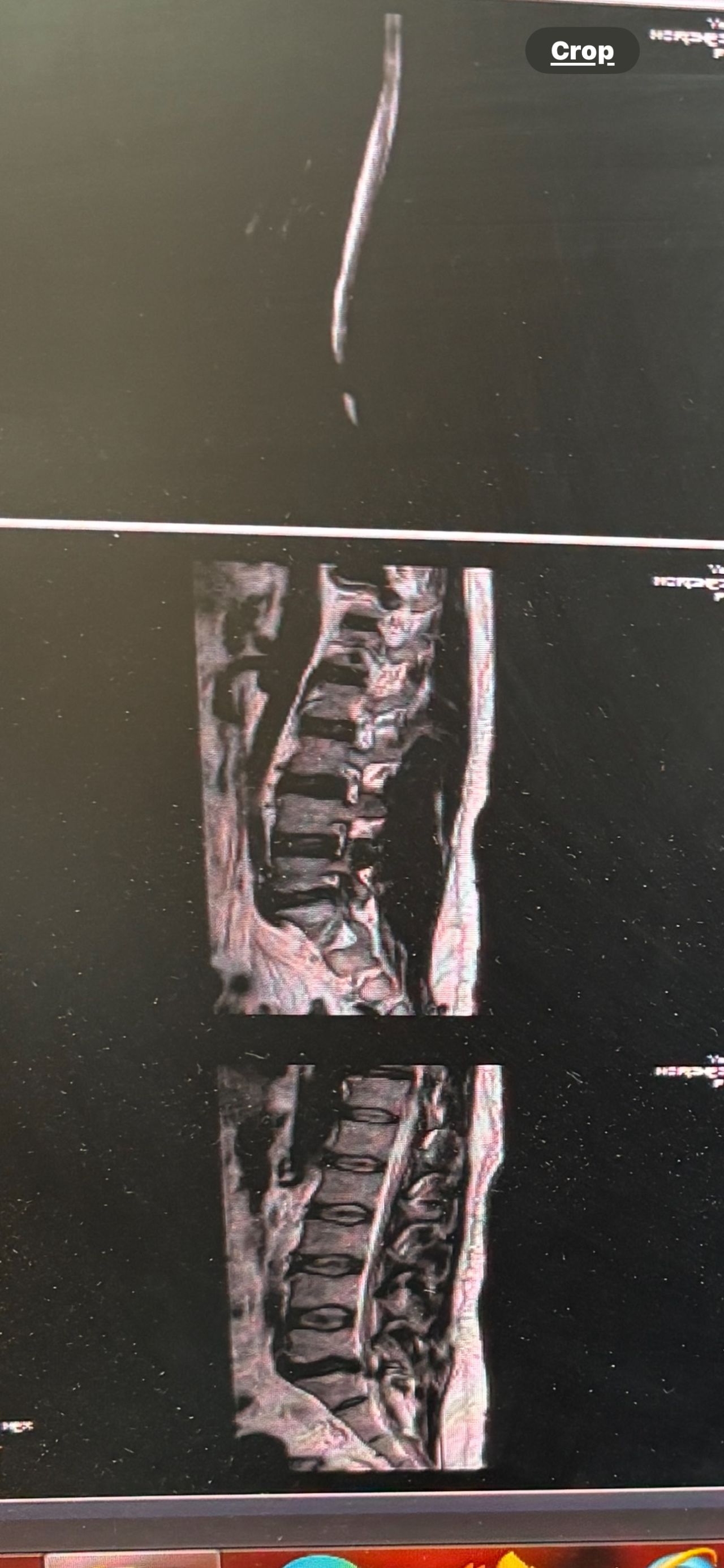
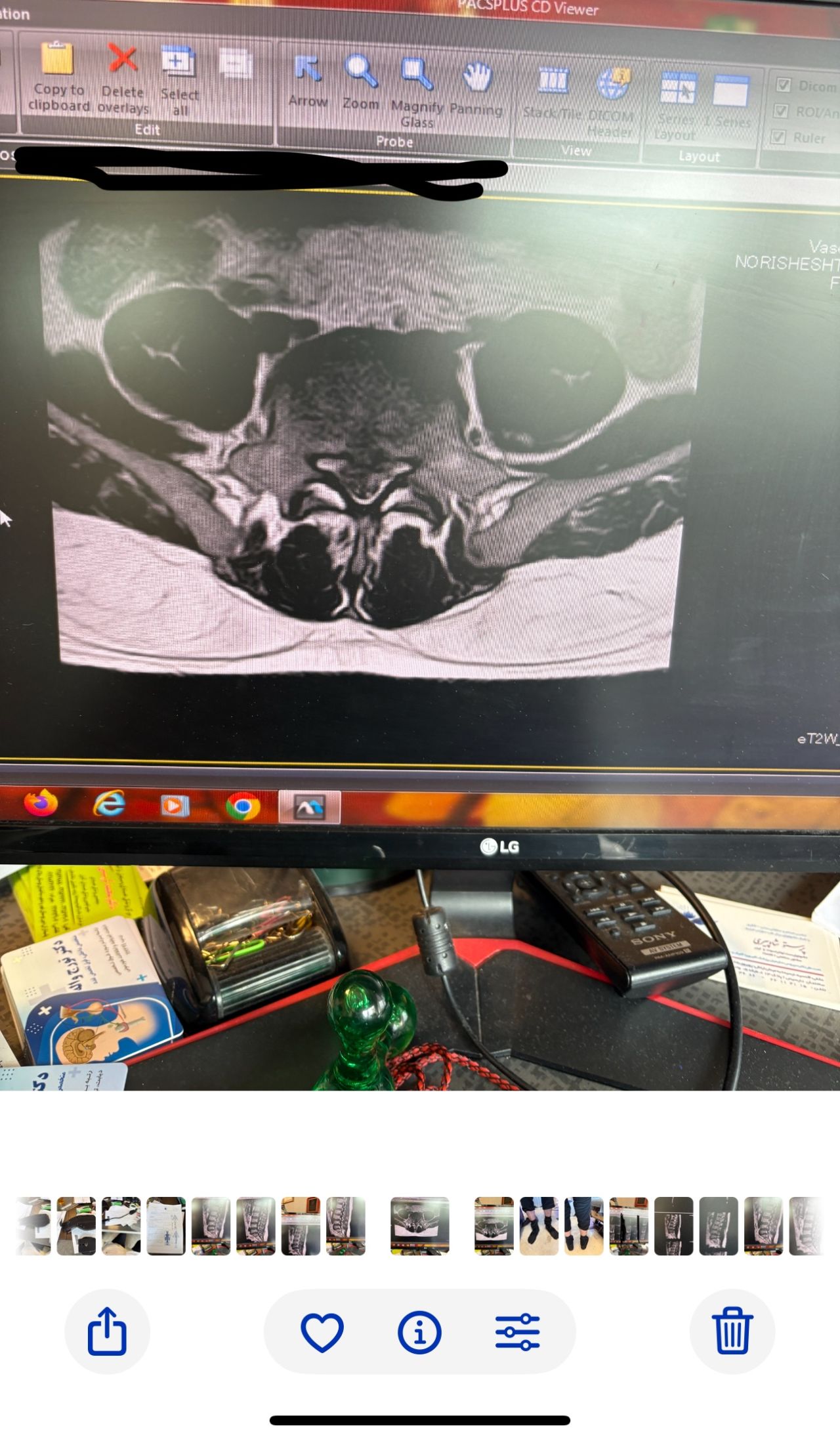
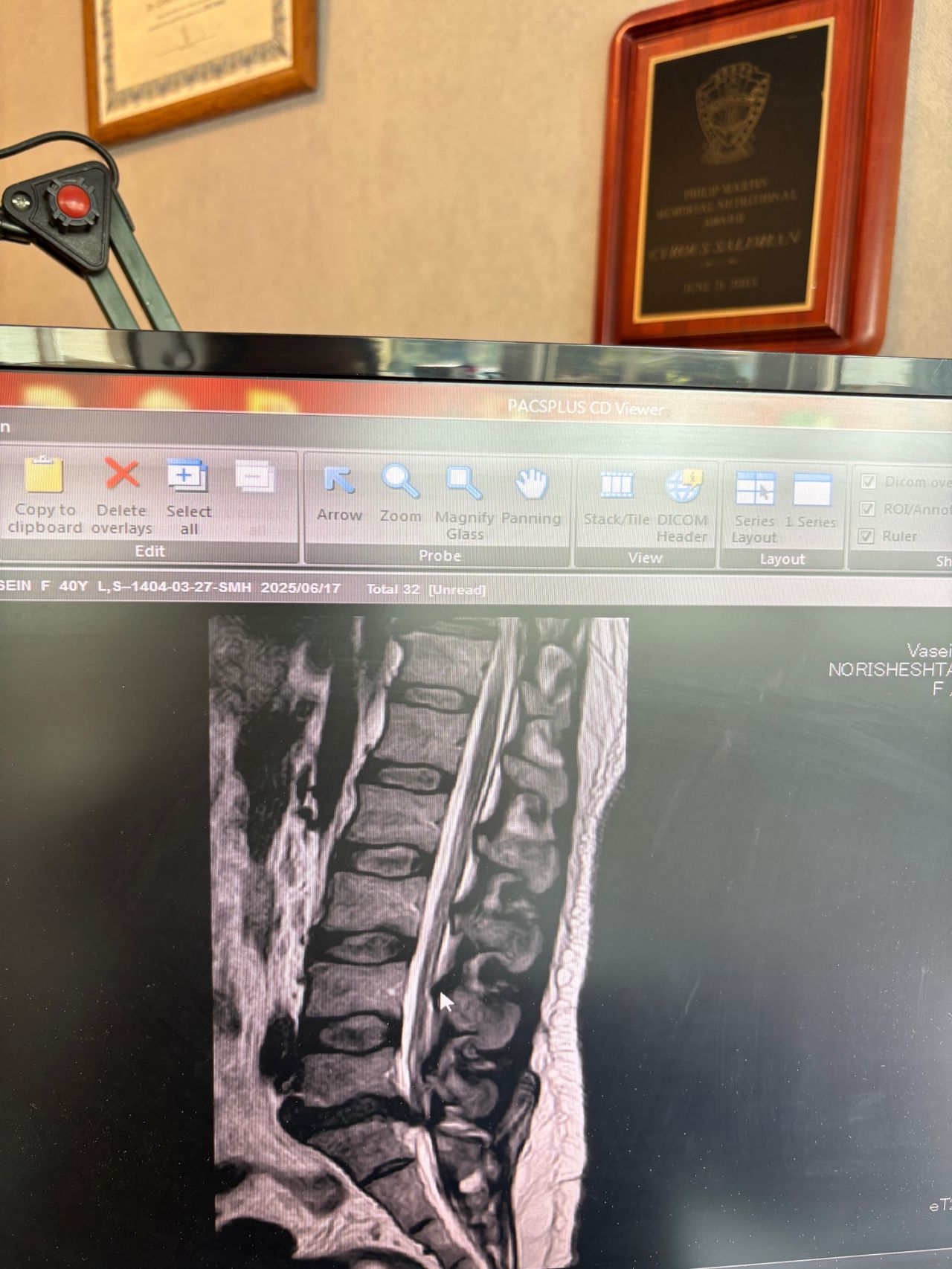
Case 5
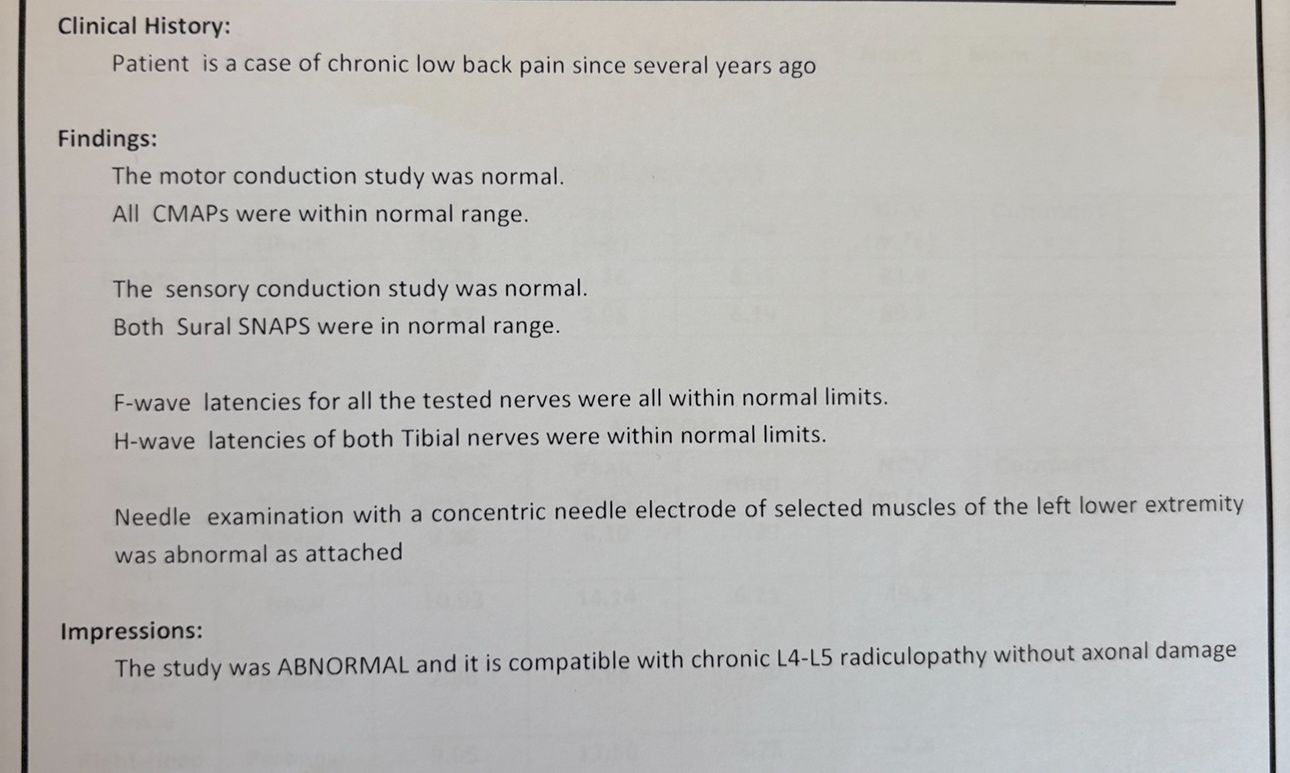
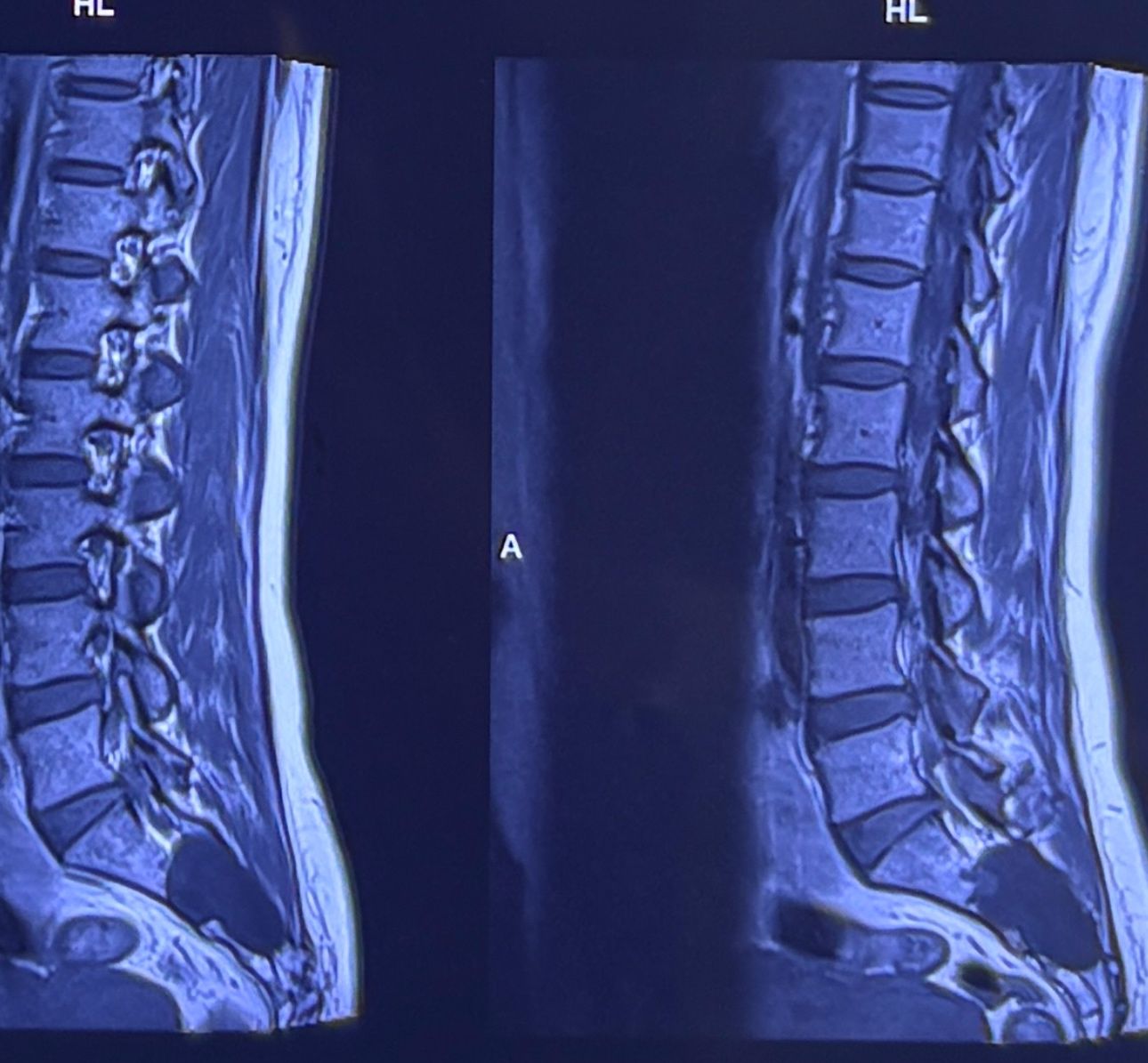
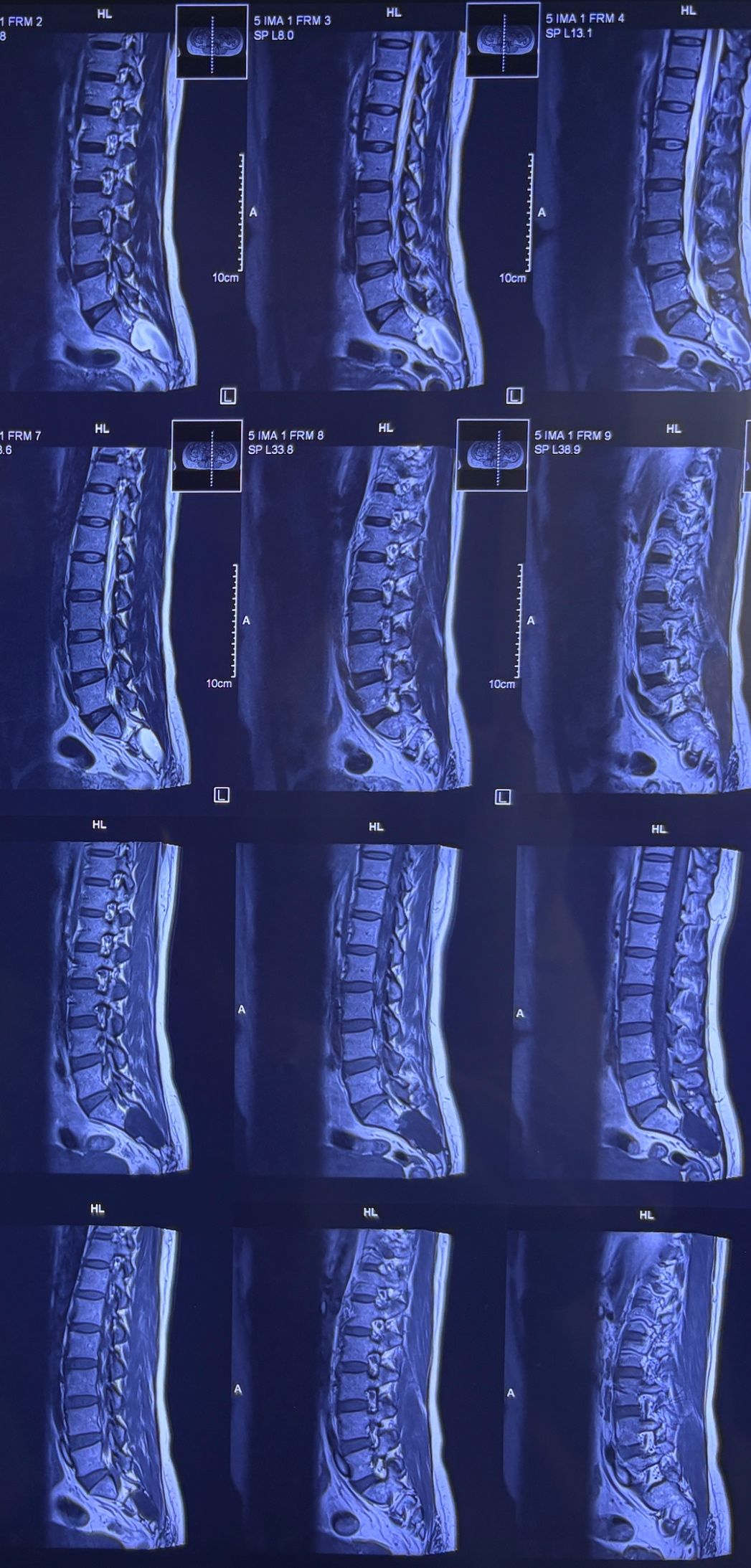
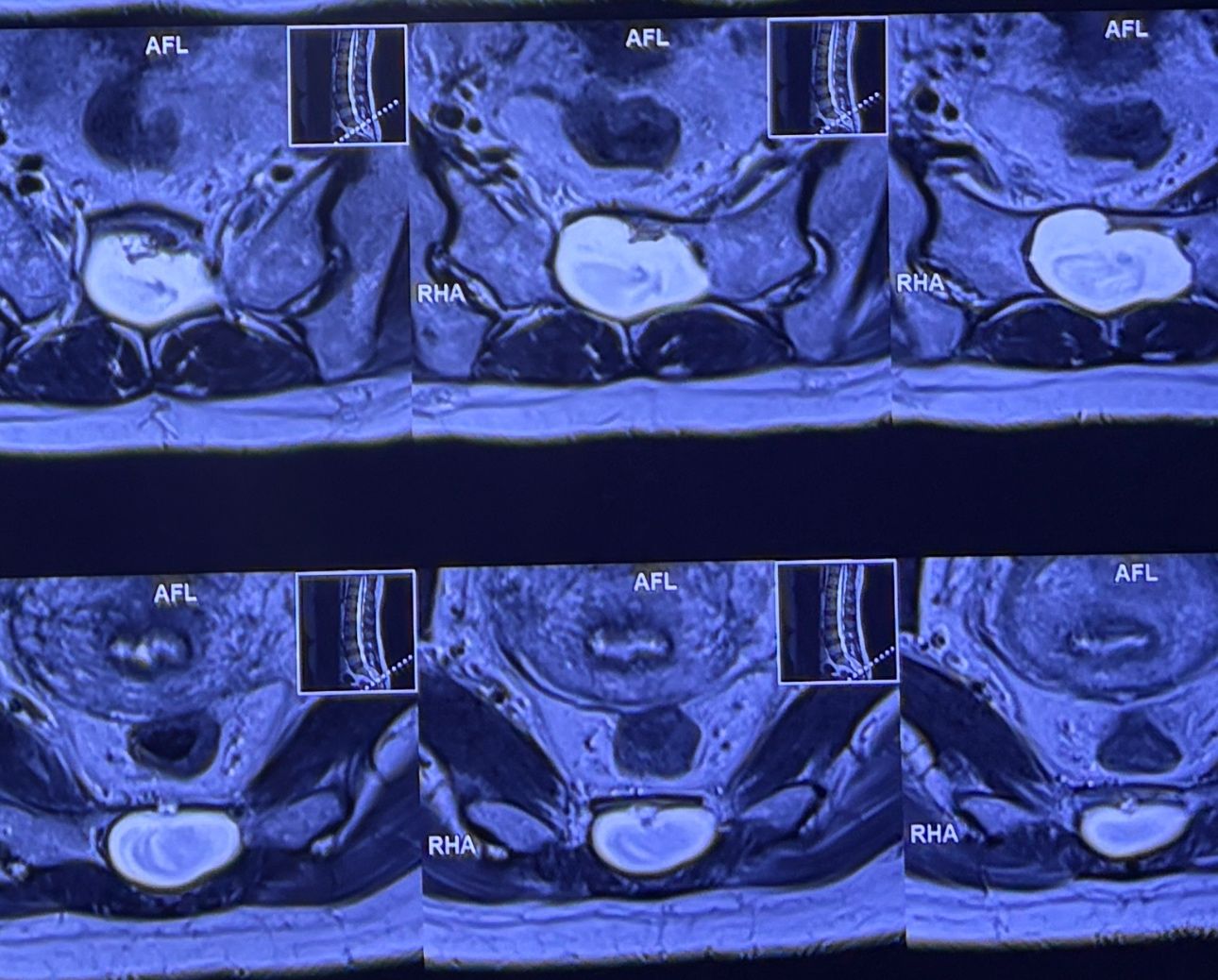
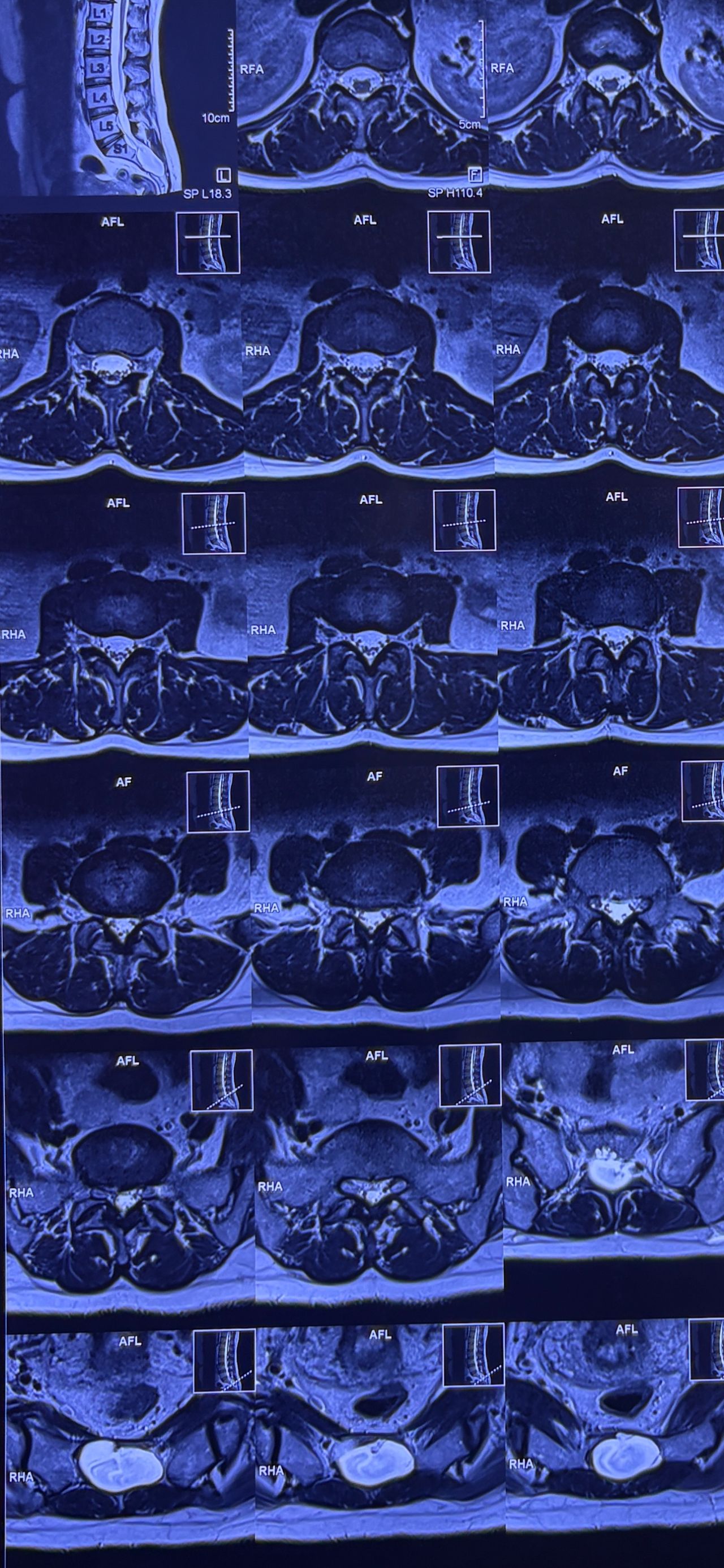
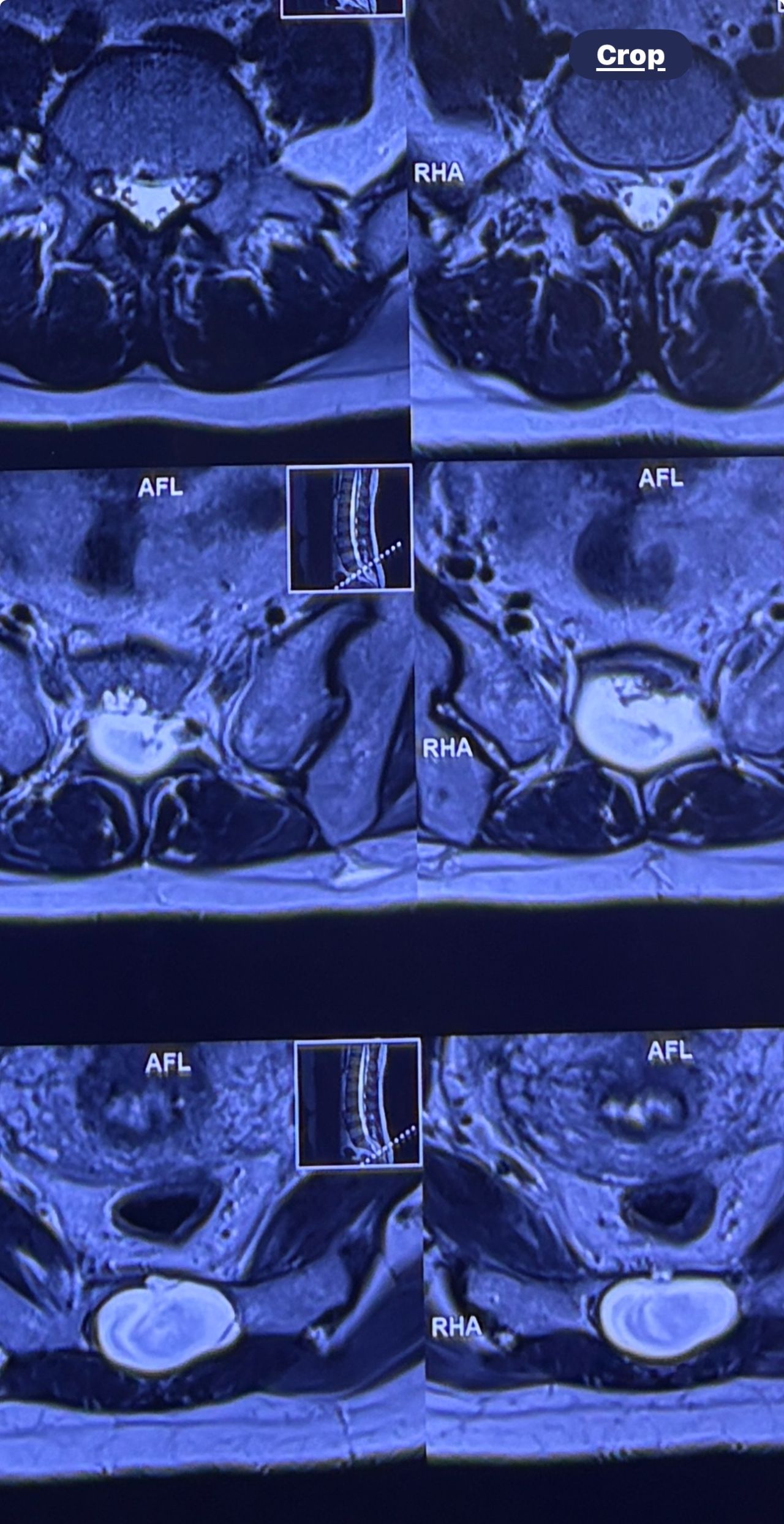
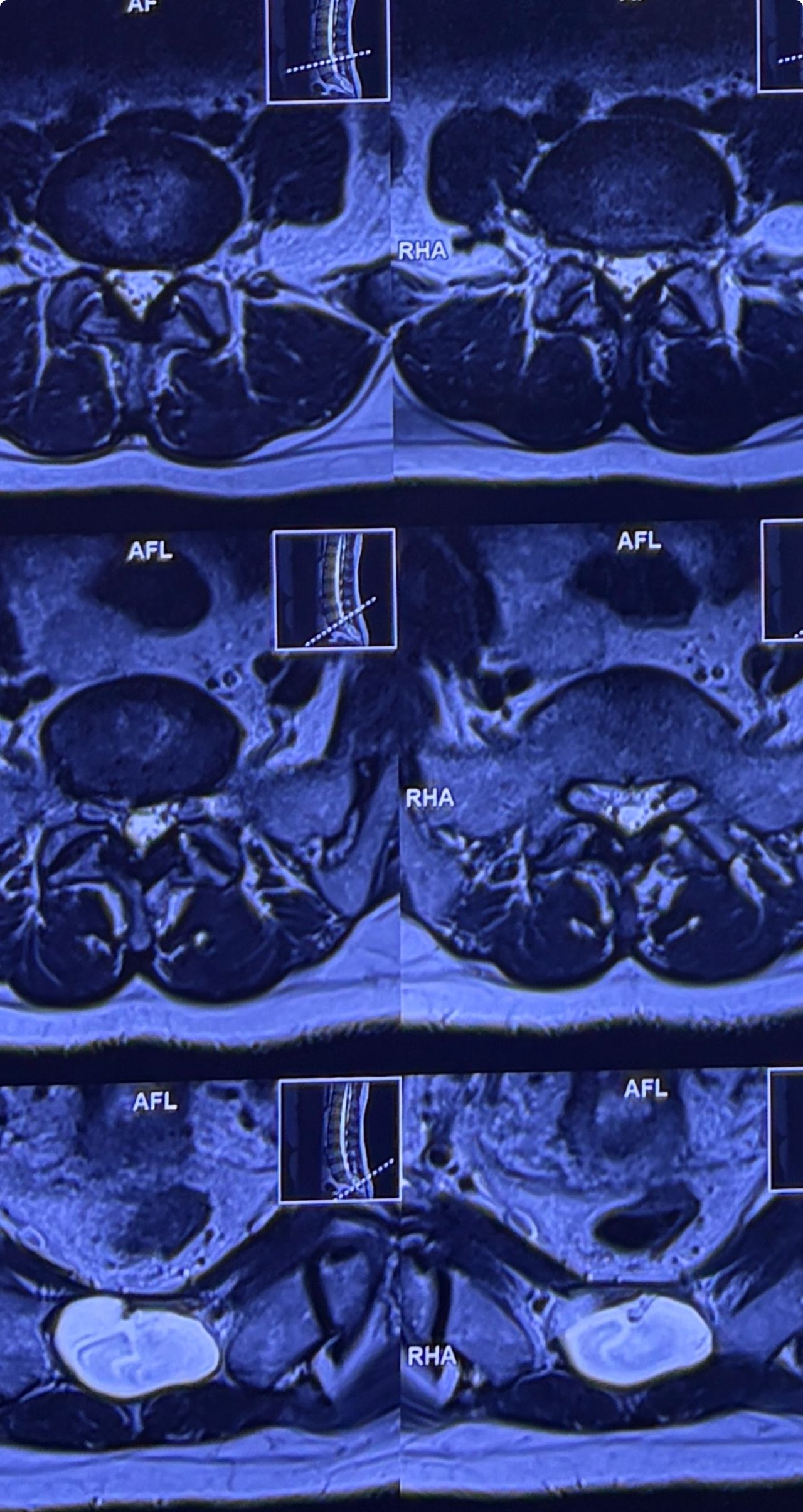
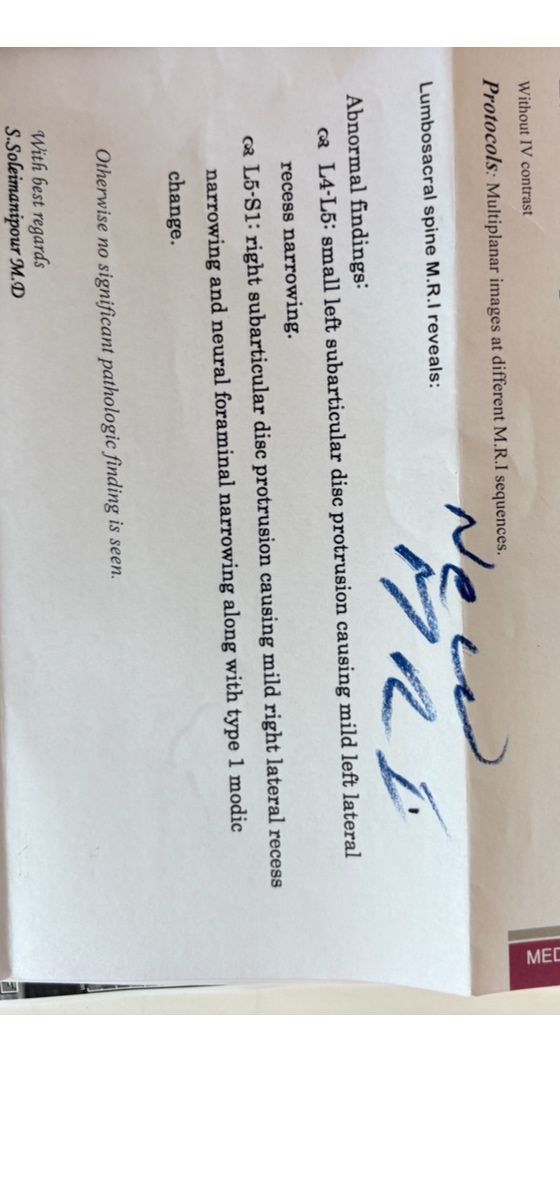
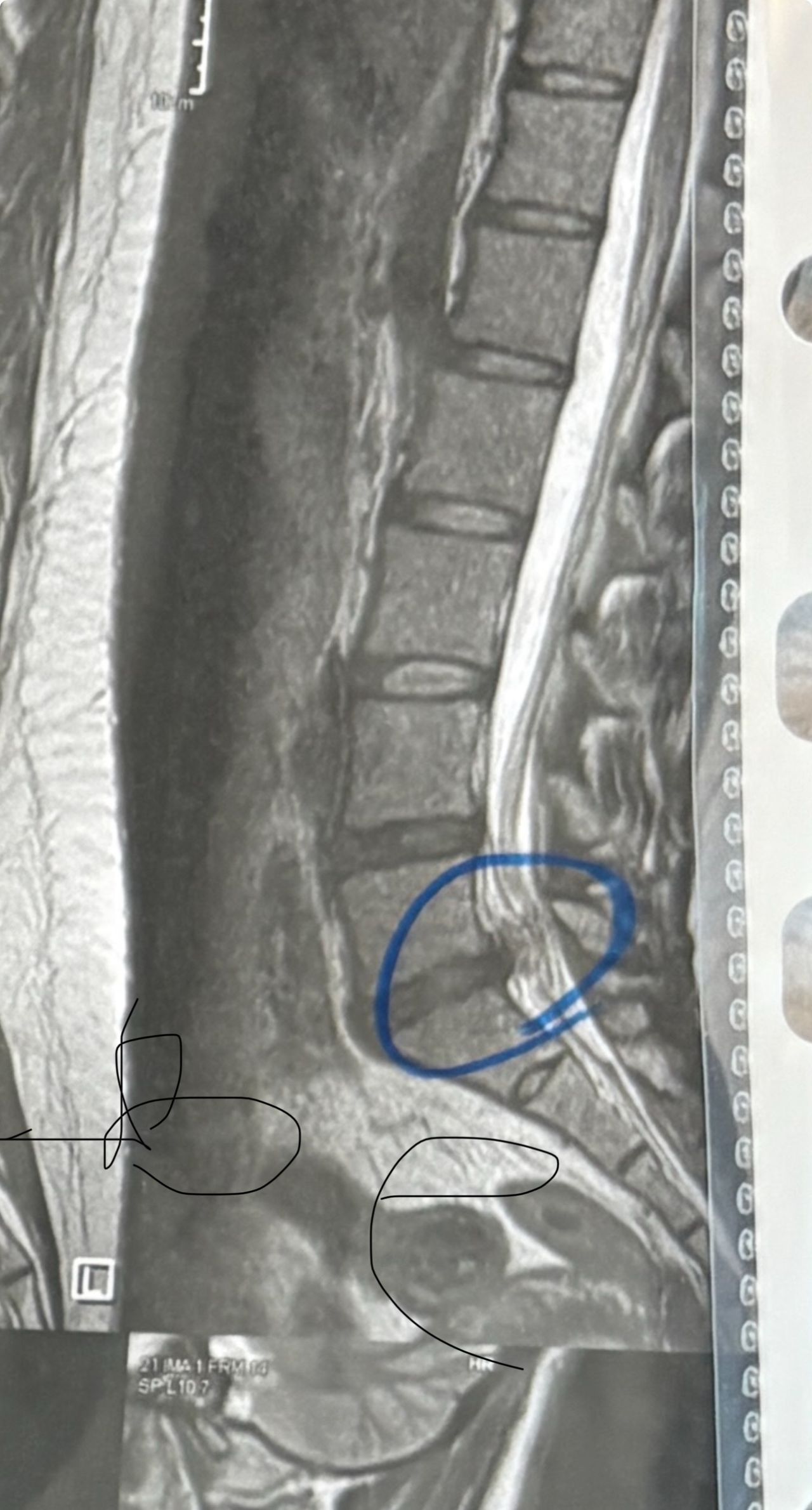
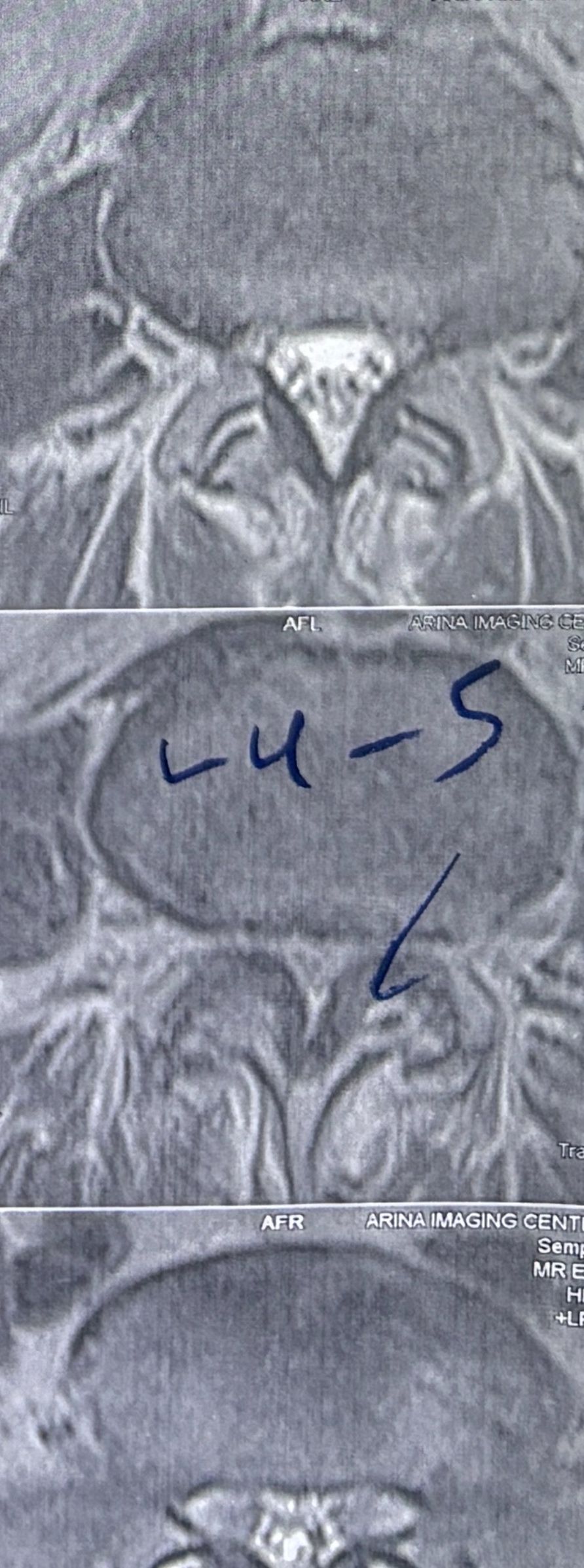
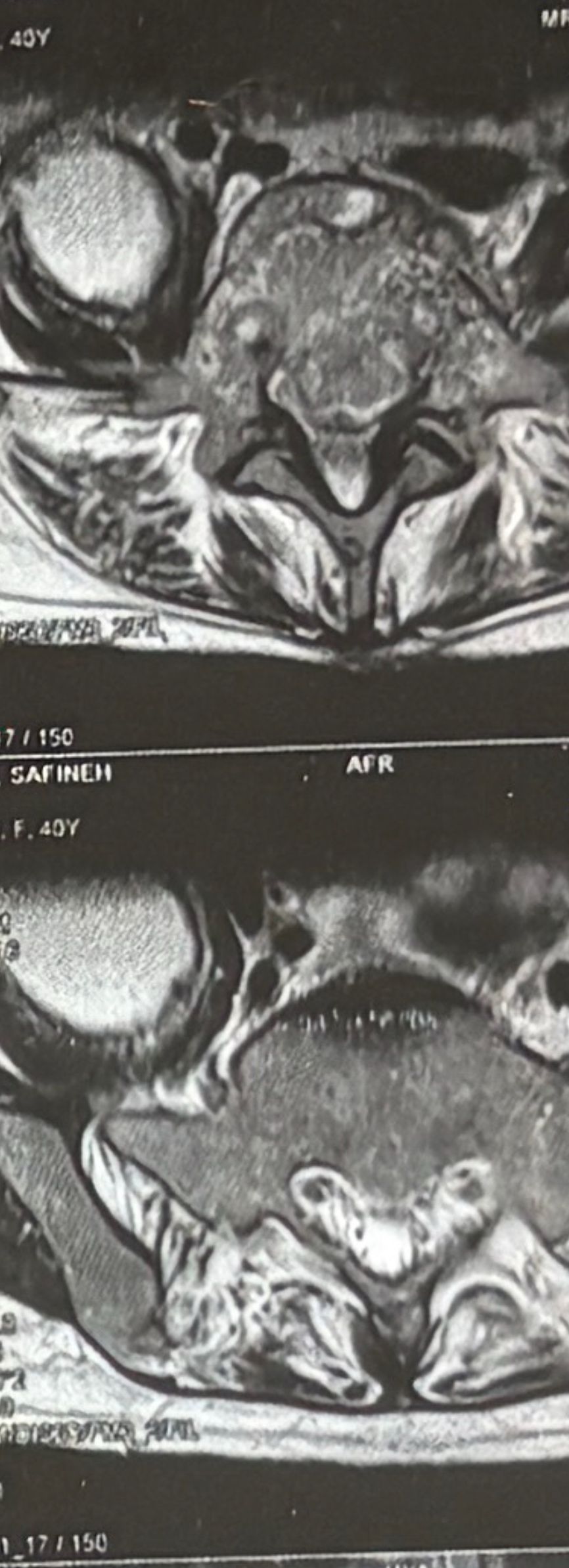
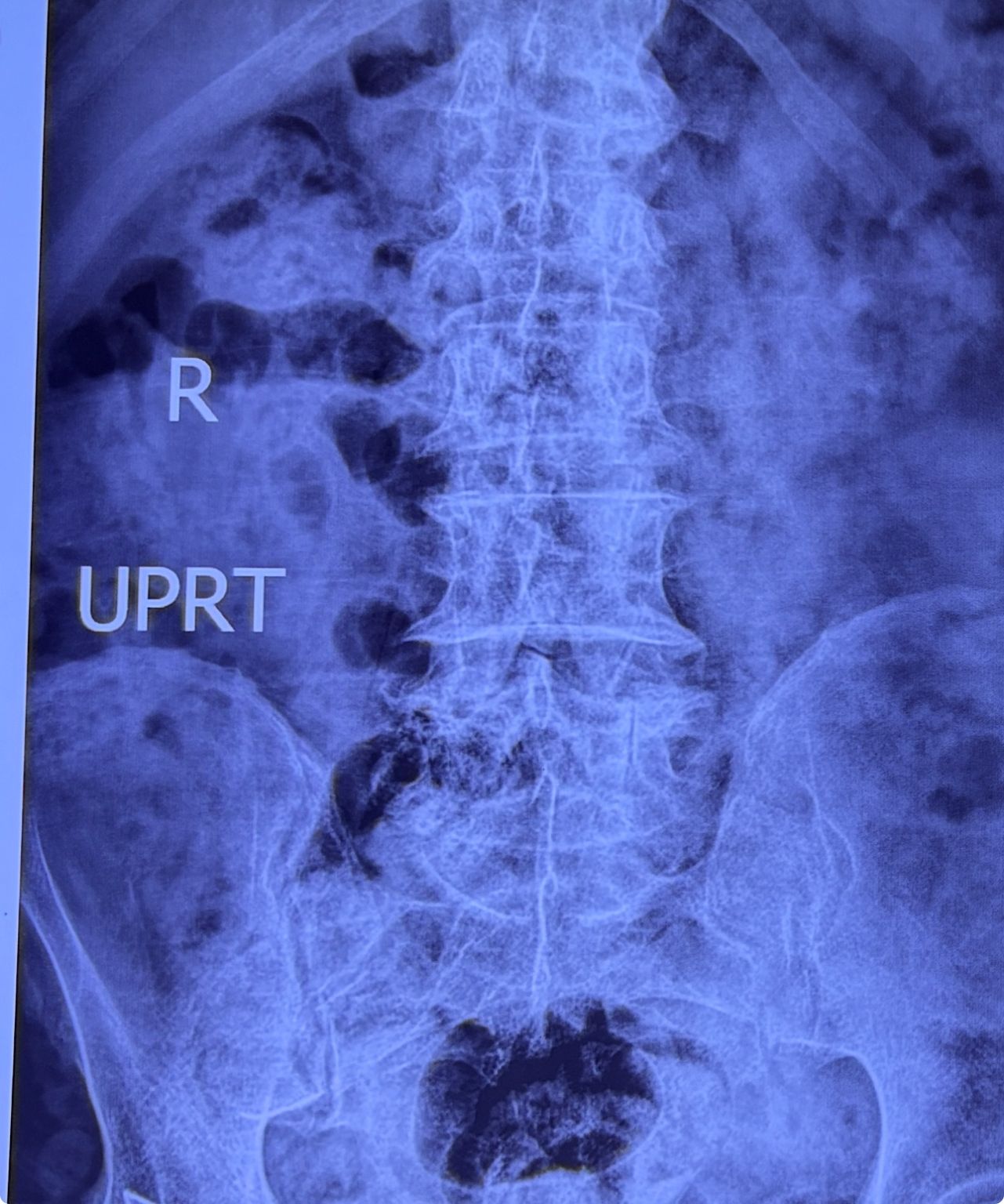
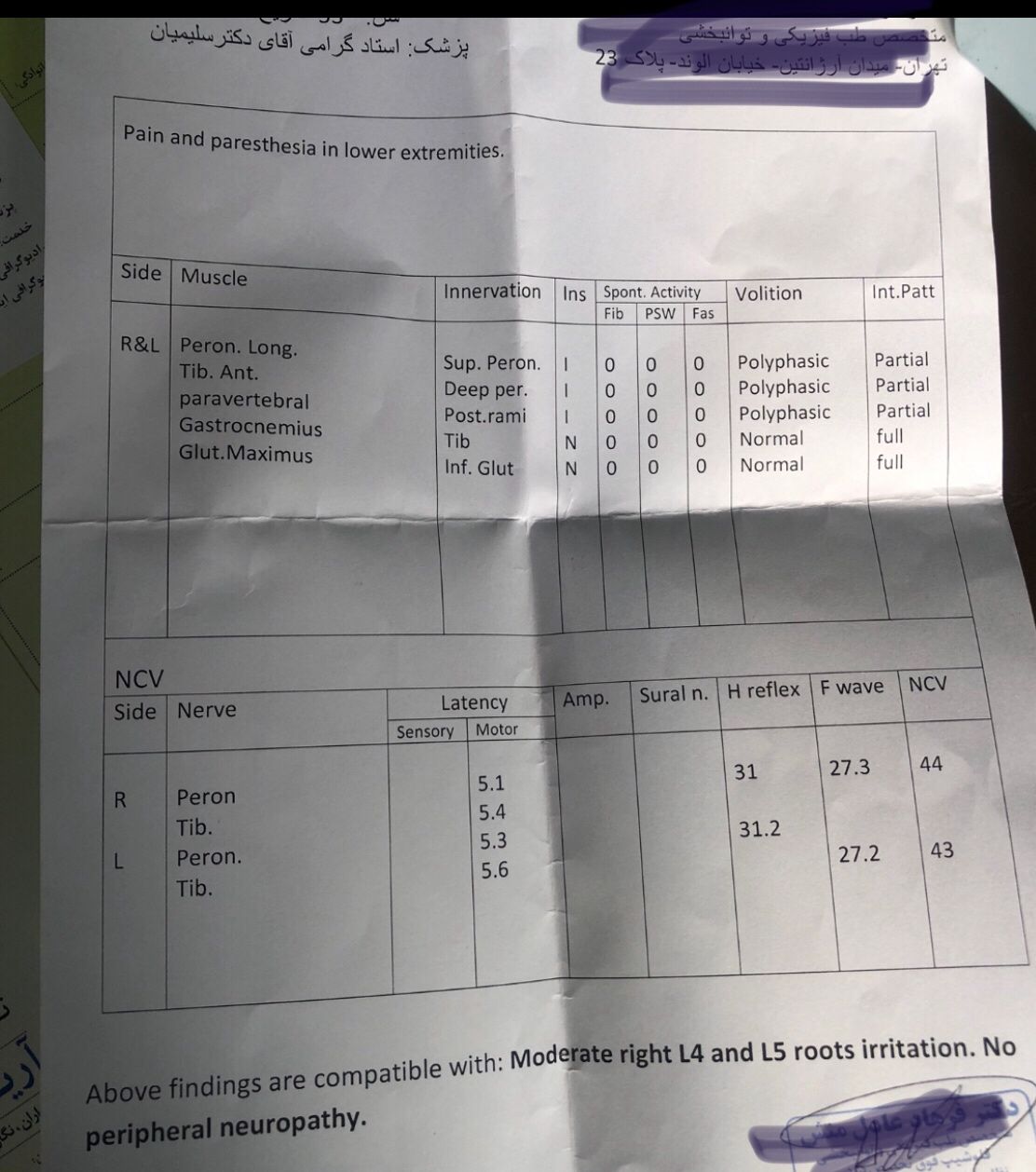
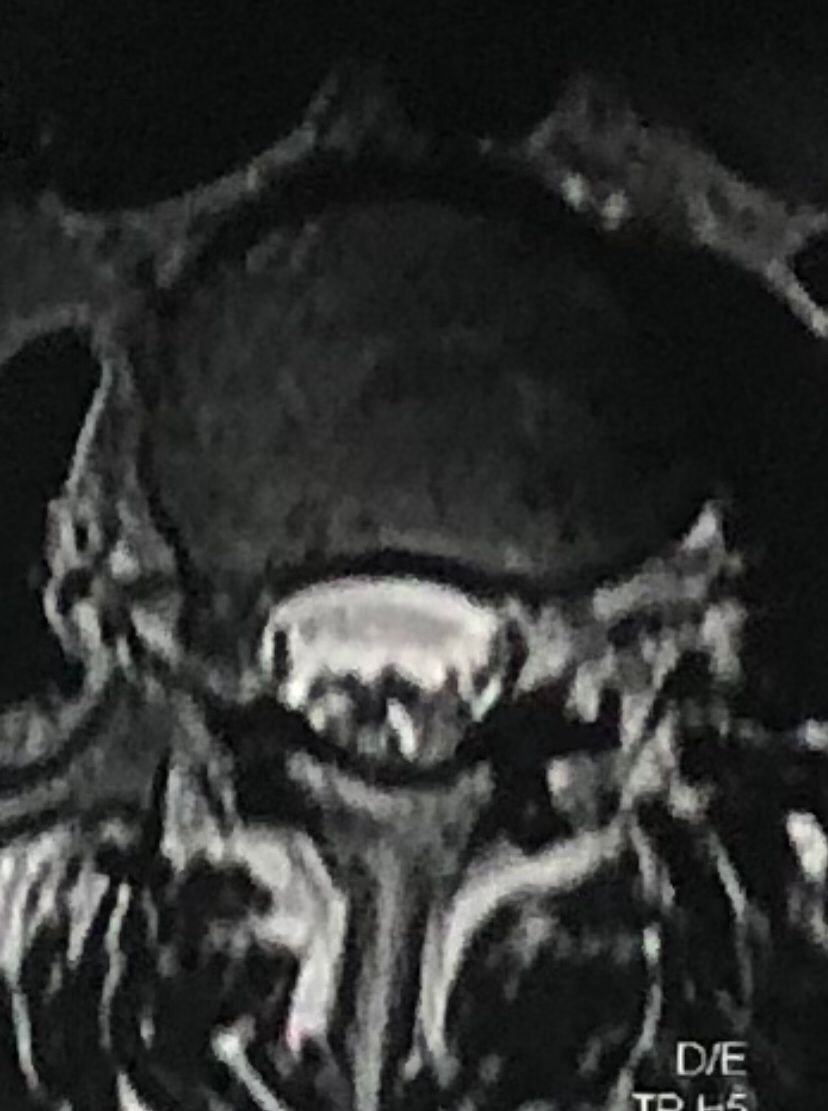
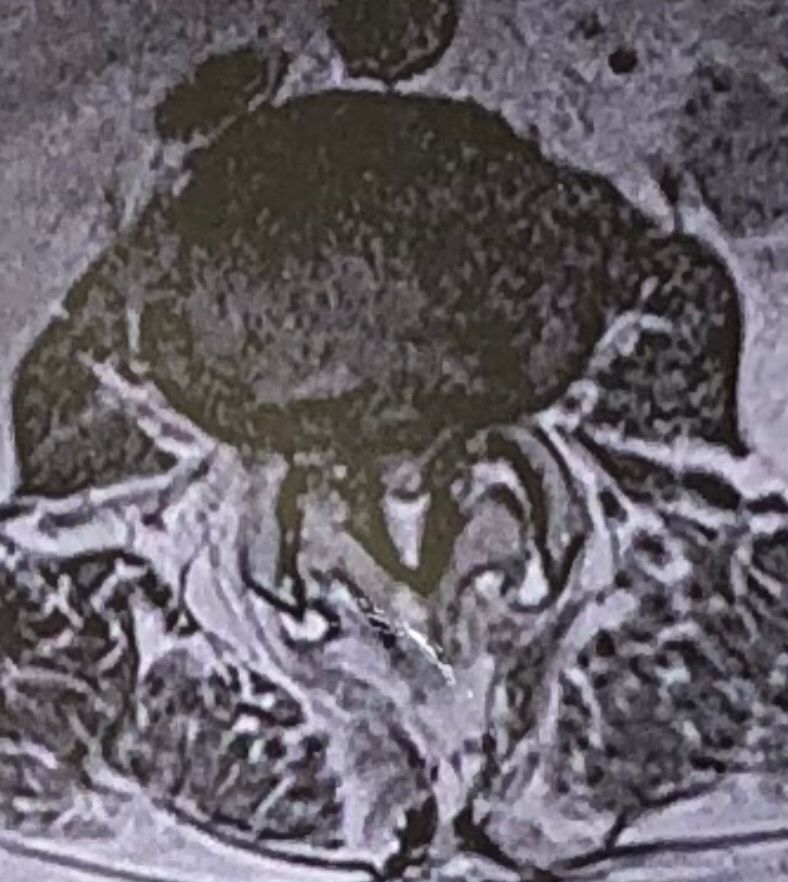
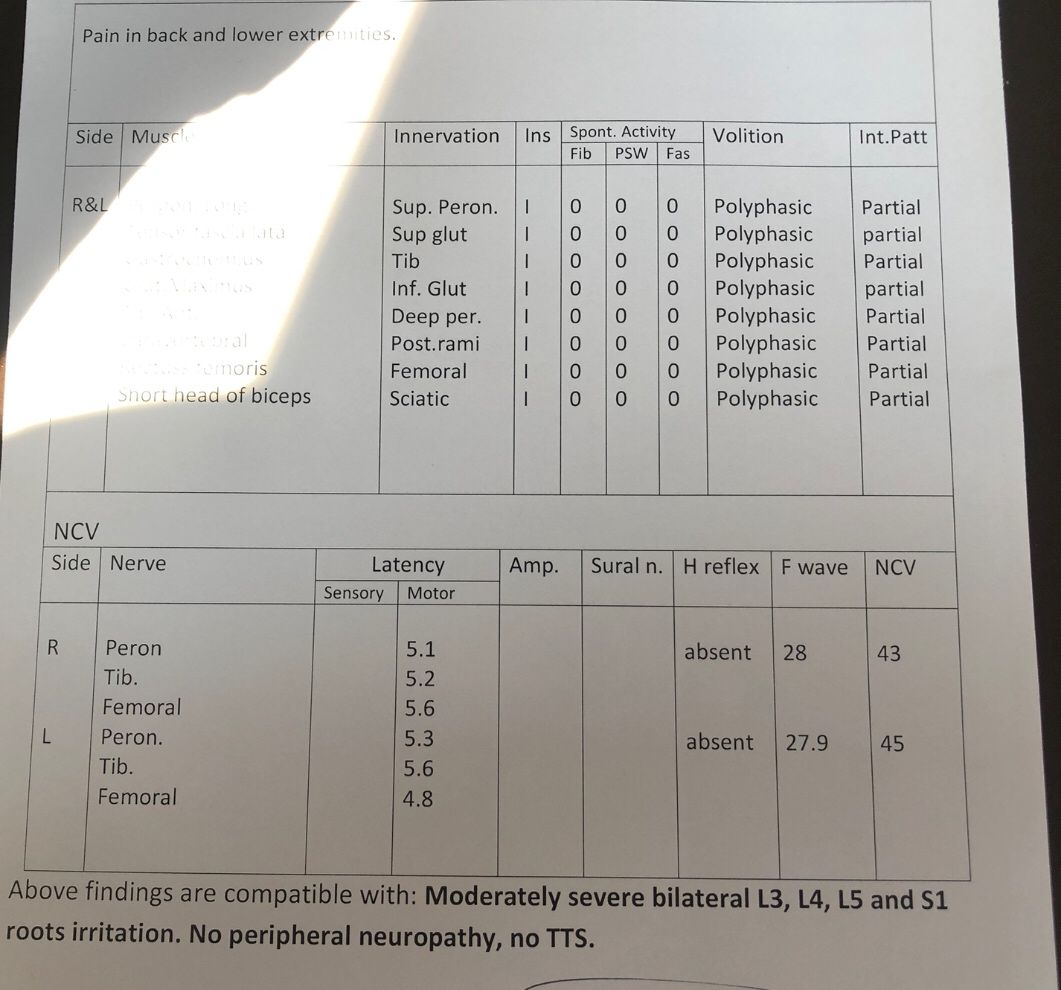
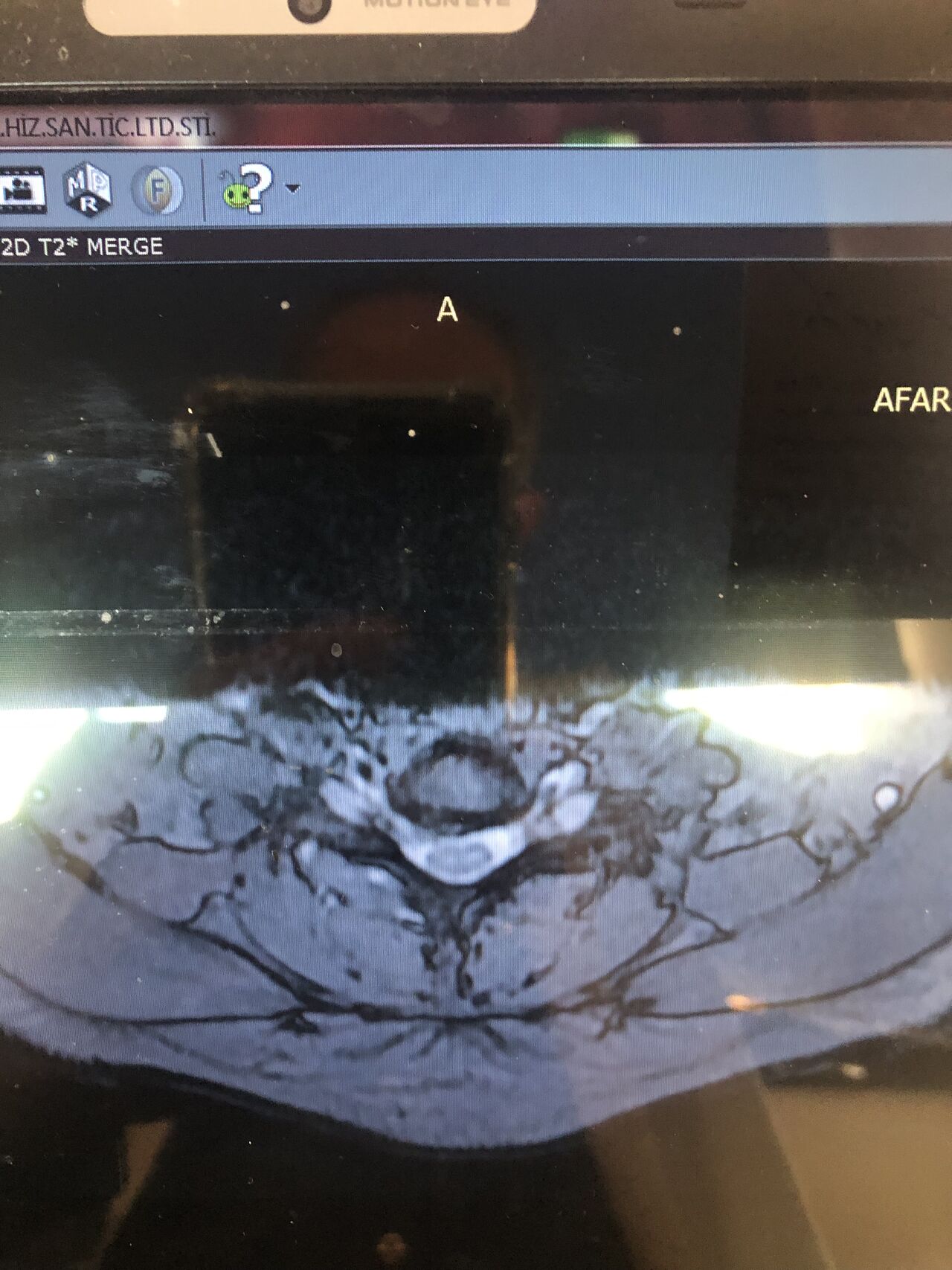
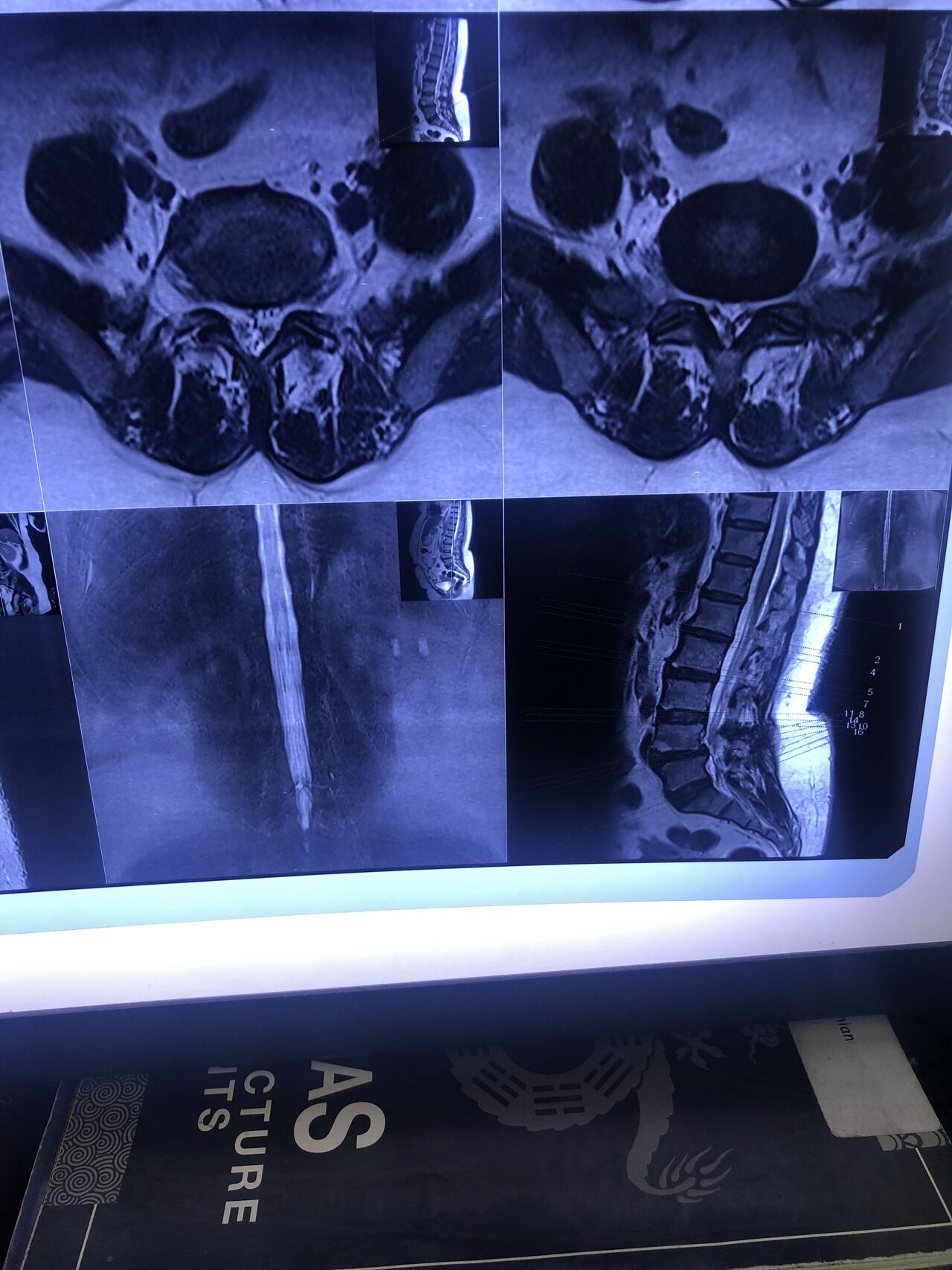
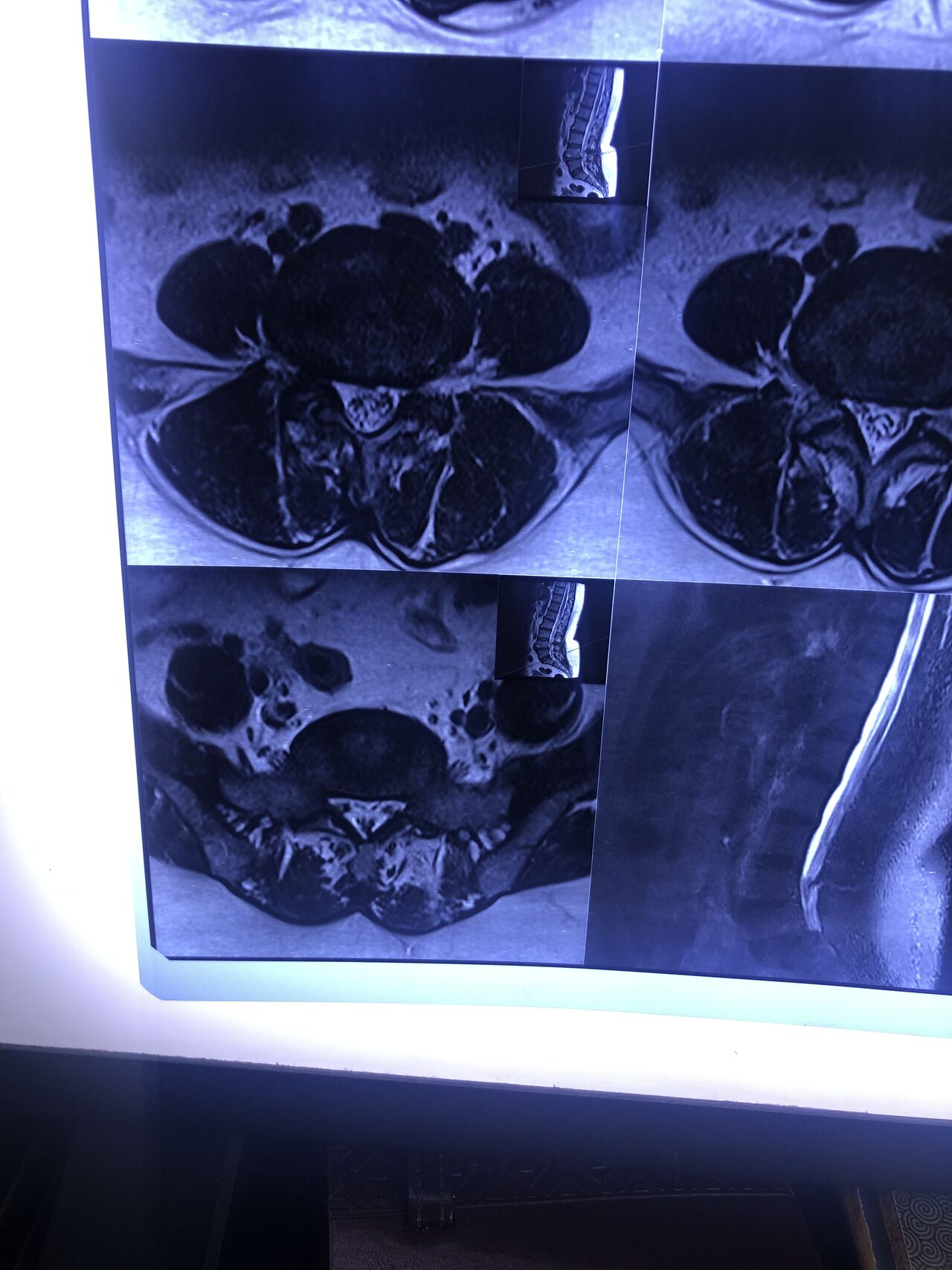
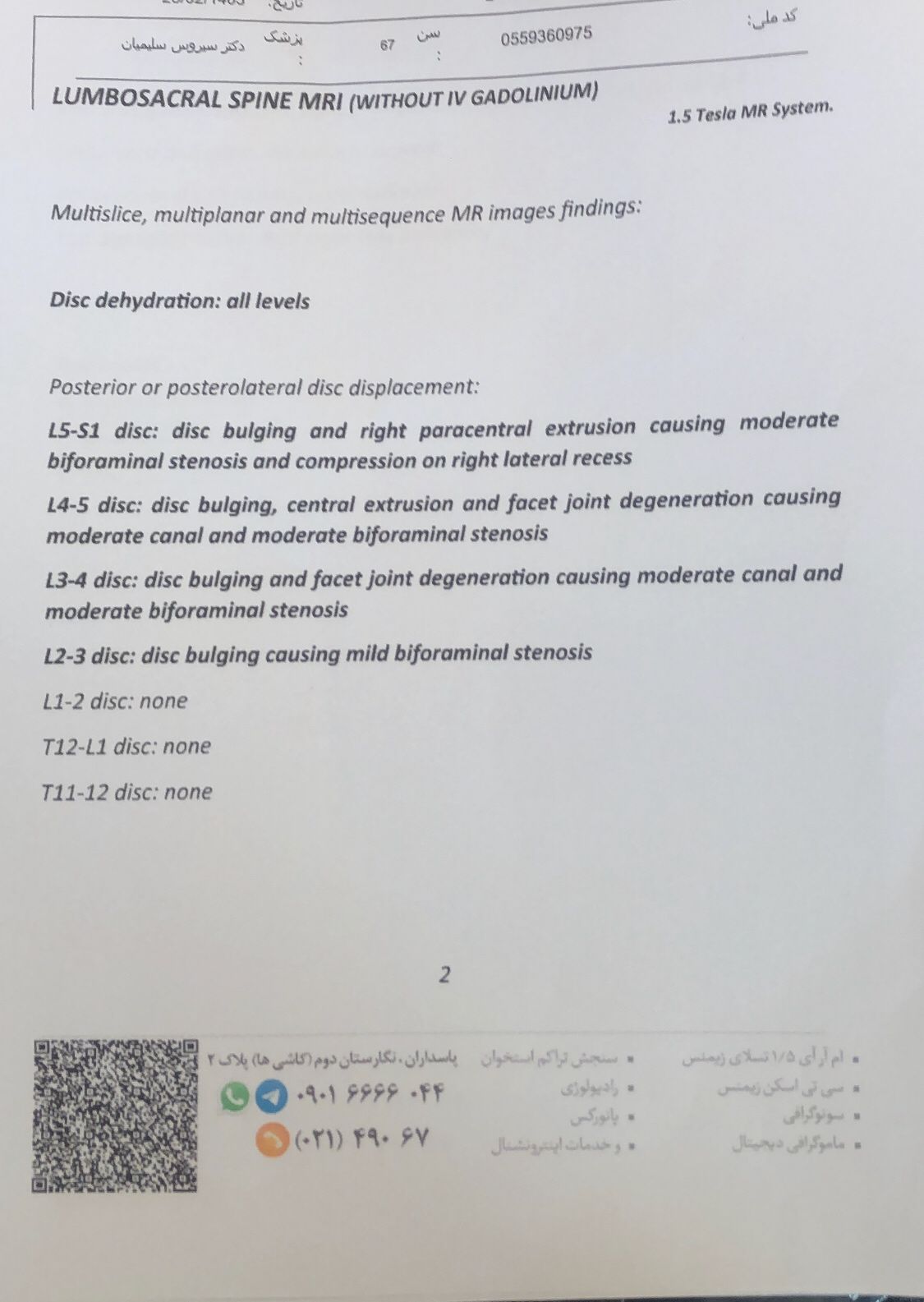
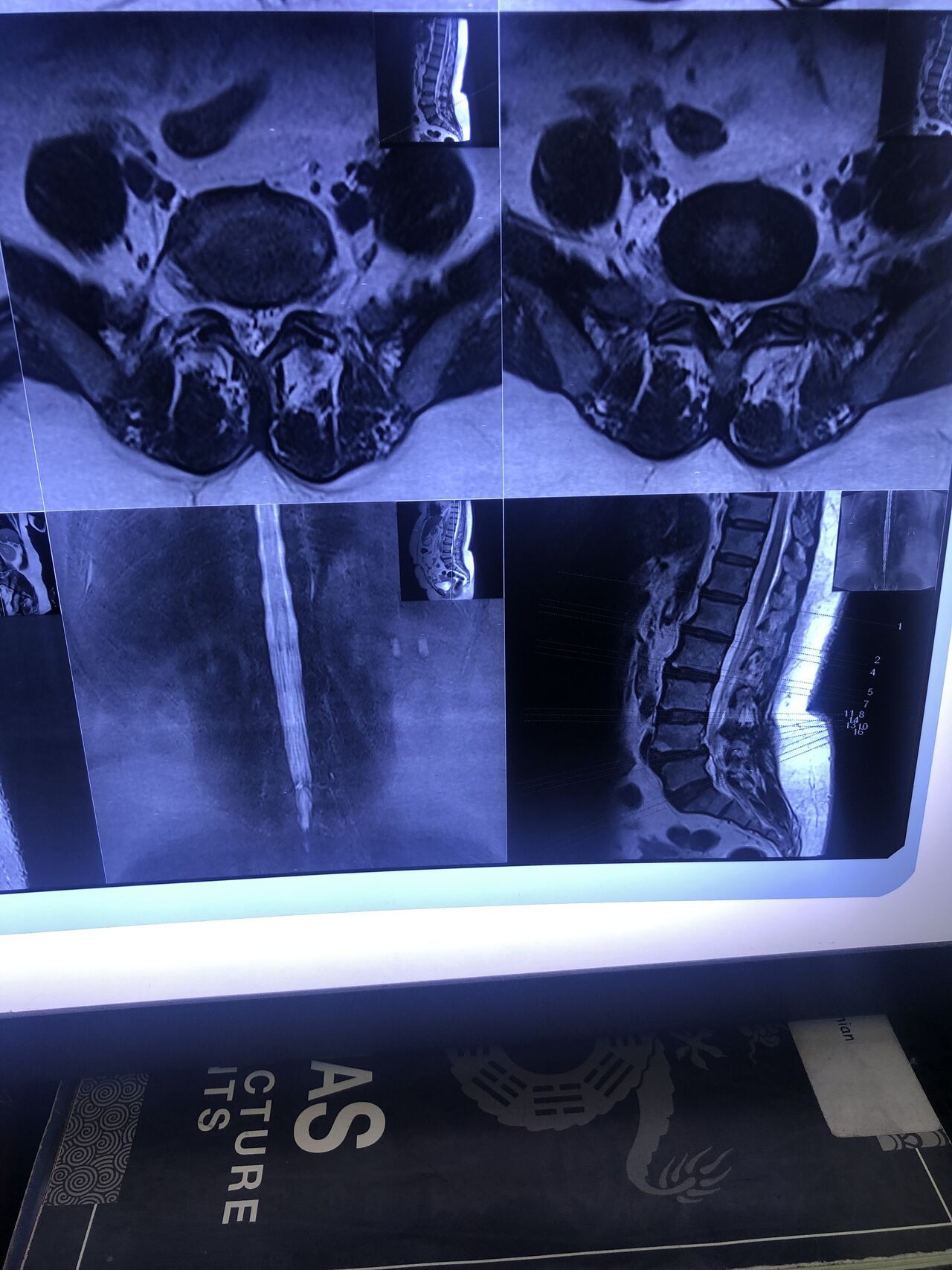
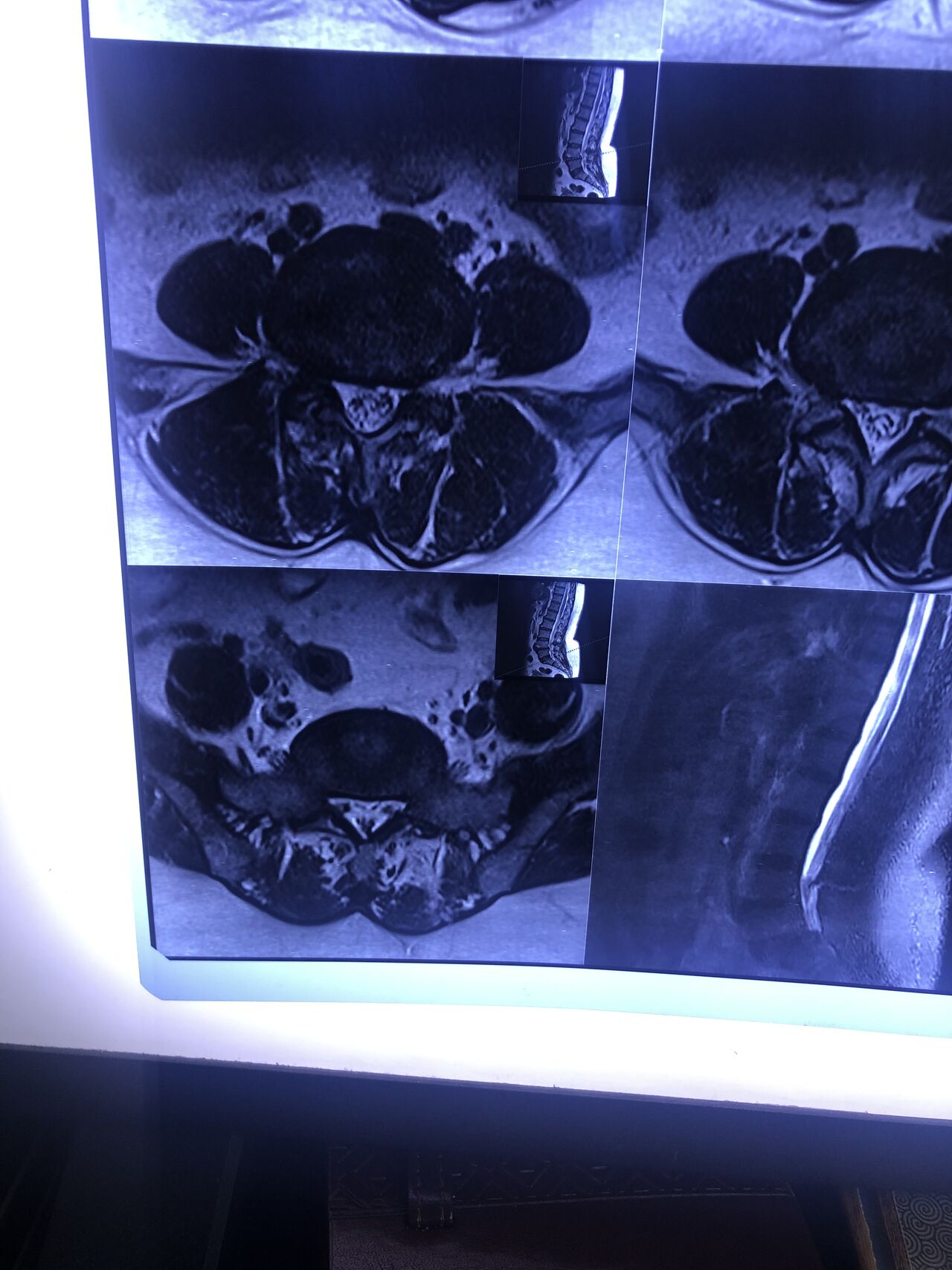
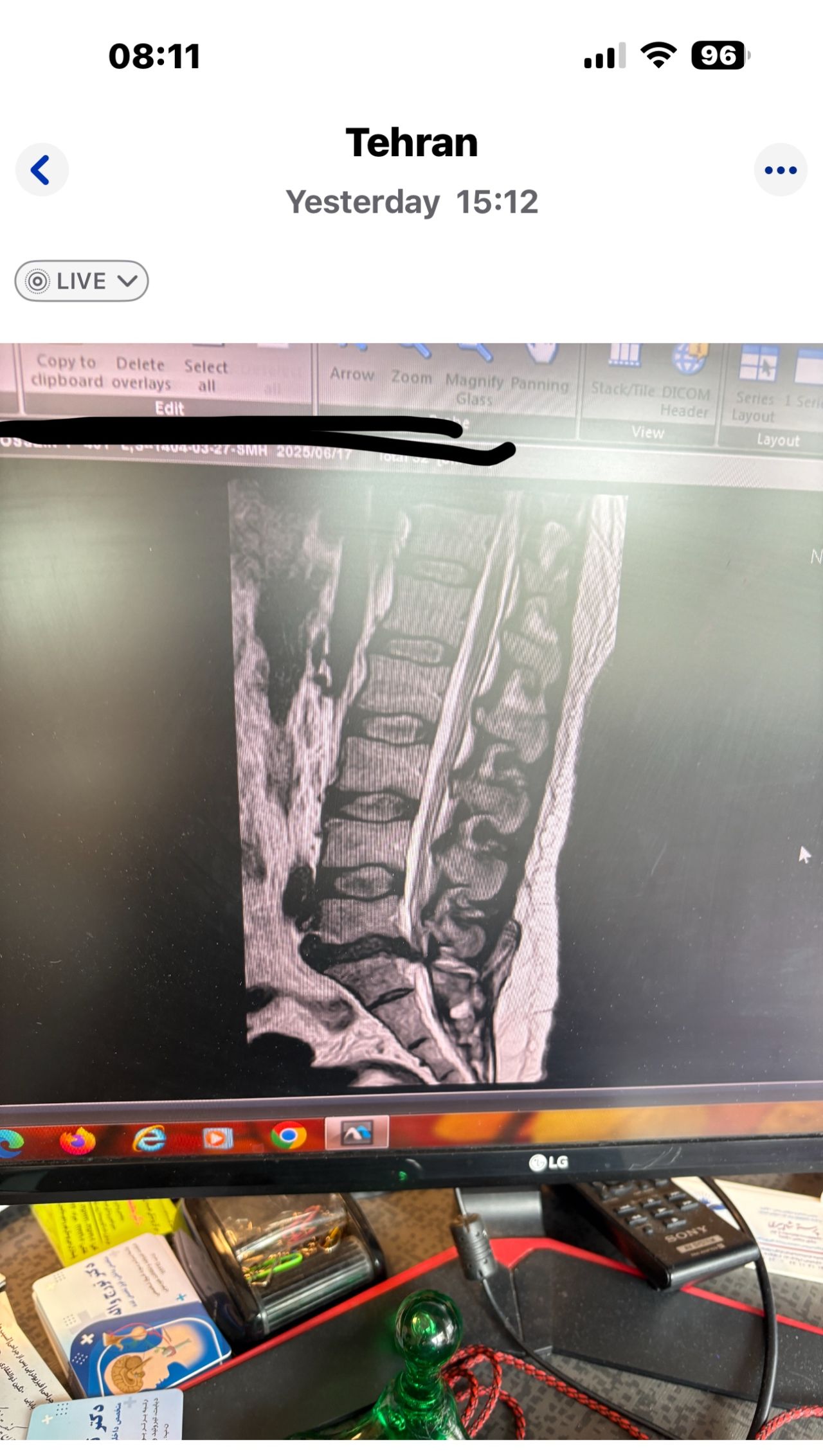
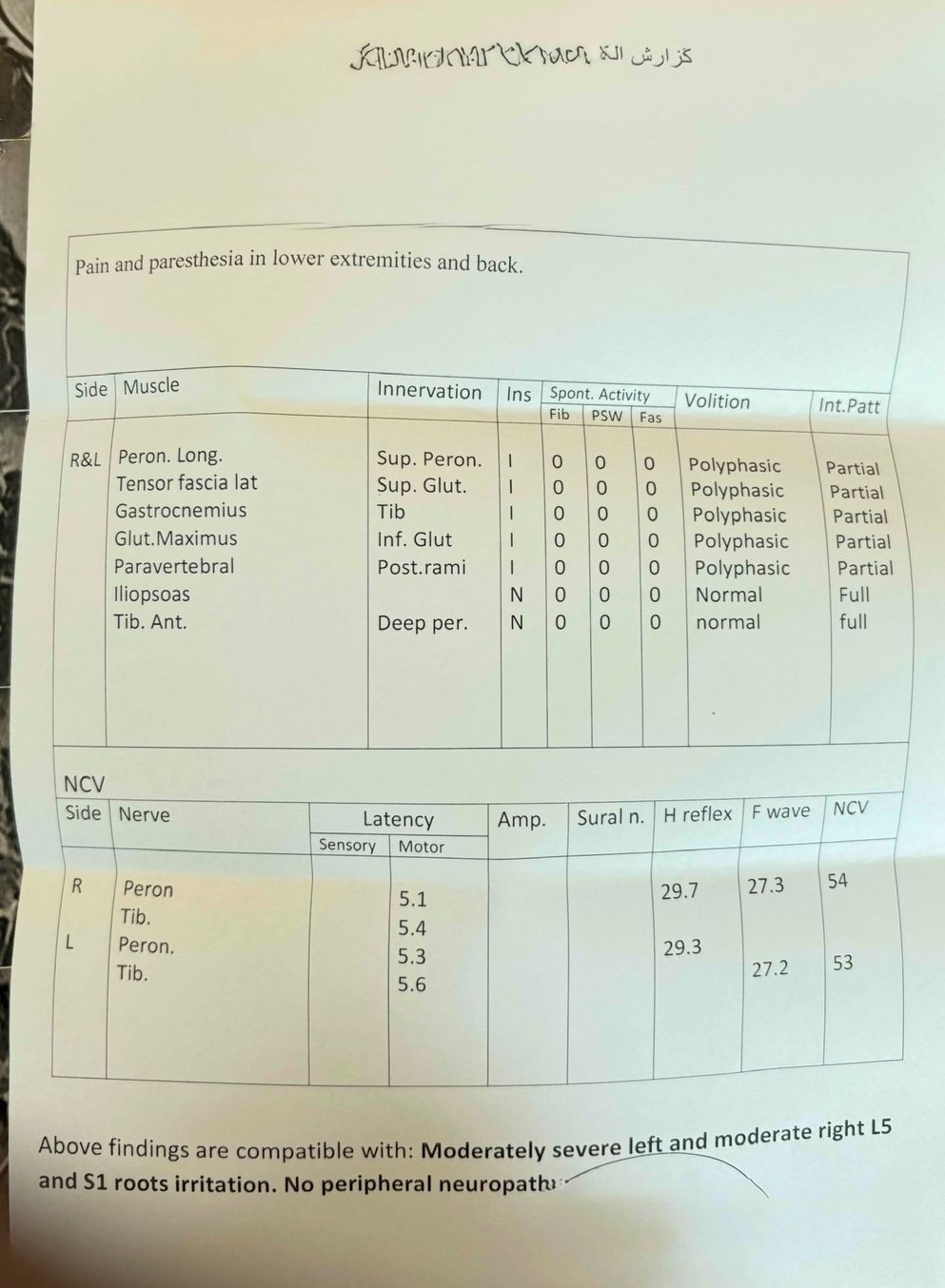
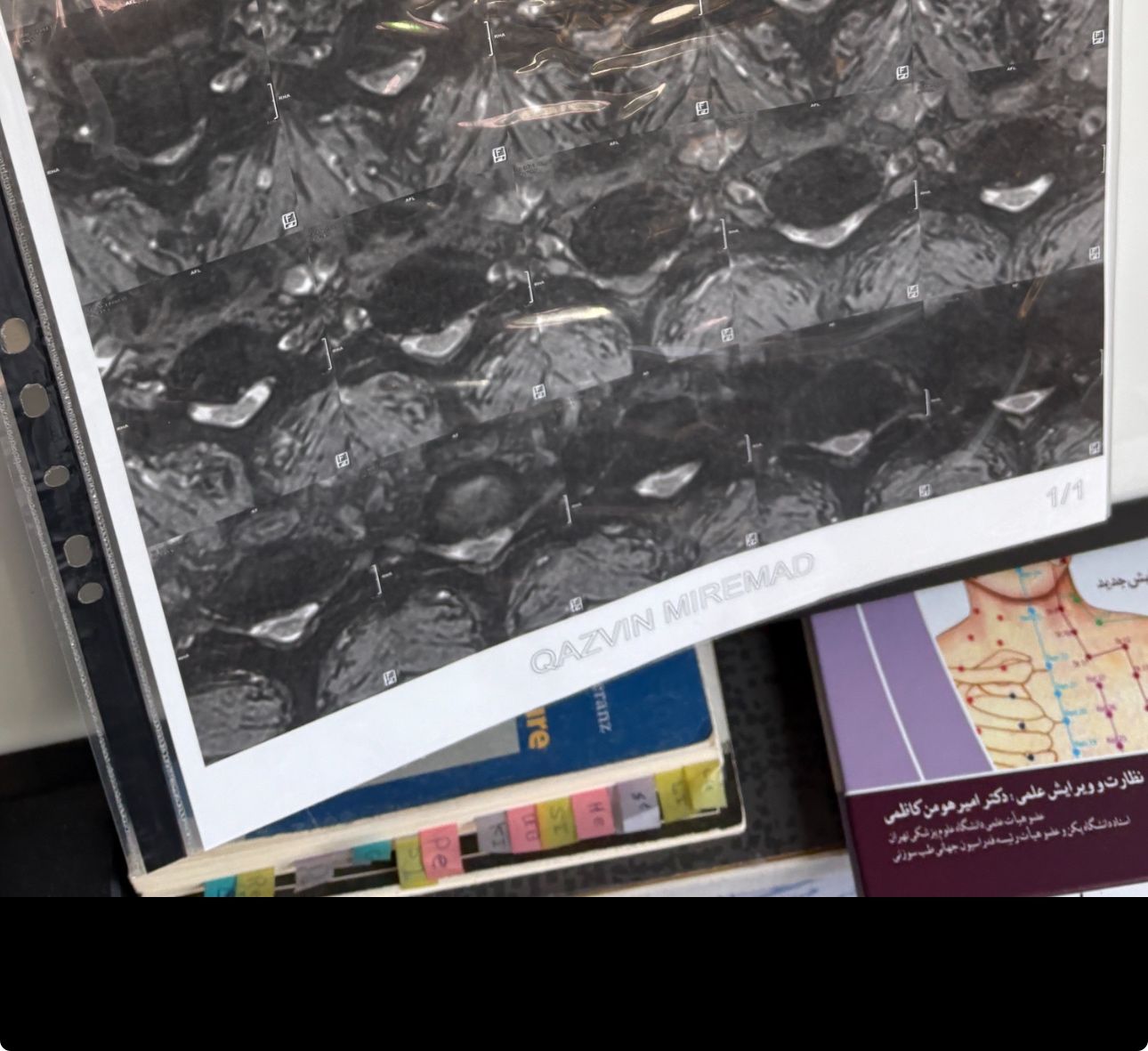
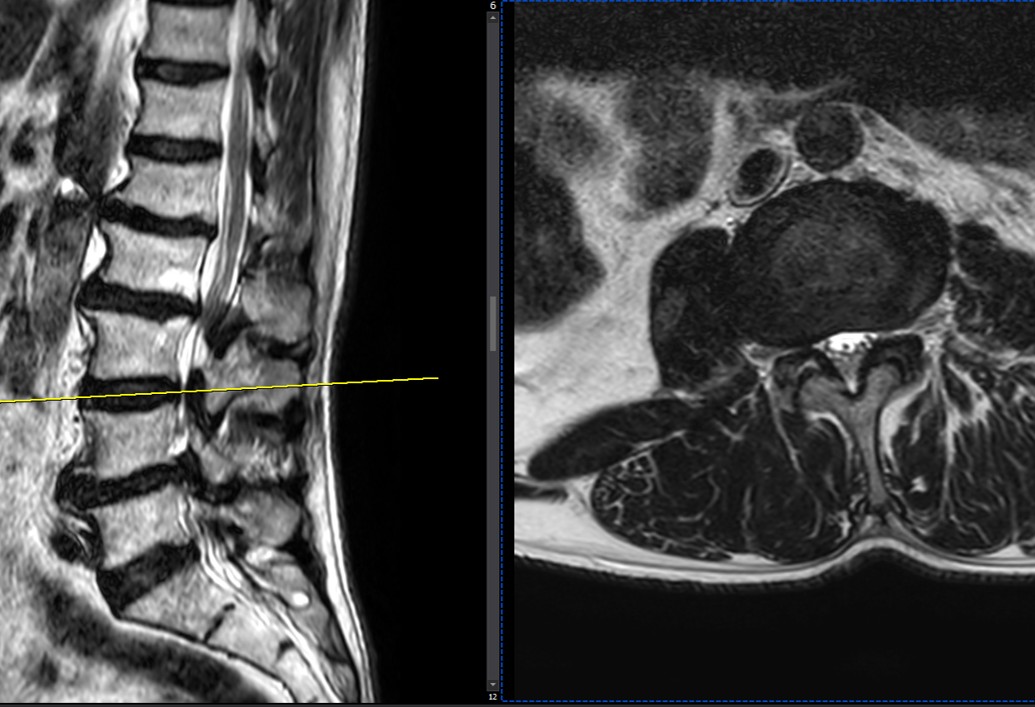
46 years old female patient presented to my clinic yesterday june 1/2025 with LBP and radicular L leg pain for several months which hasn’t responded to physio 2 neurosurgeons have visited her and didn’t suggest any surgery Neurological exam was unremarkable please see her mri/ emg/ncv and her huge tarlov cyst and possible L IVF L4-5 hyperbulge I ordered sacrum mri and ct scan and new emg/ncv and asked her with her sacral Ct scan and MRI first sees another two famous neurosurgeons and see if that large cyst is the reason for her pain if not i can work on her L4-S1 area Do you think her radicular pain can originate from her large cyst in sacrum? Do you consider surgery and removing her sacral cyst?
Case 6
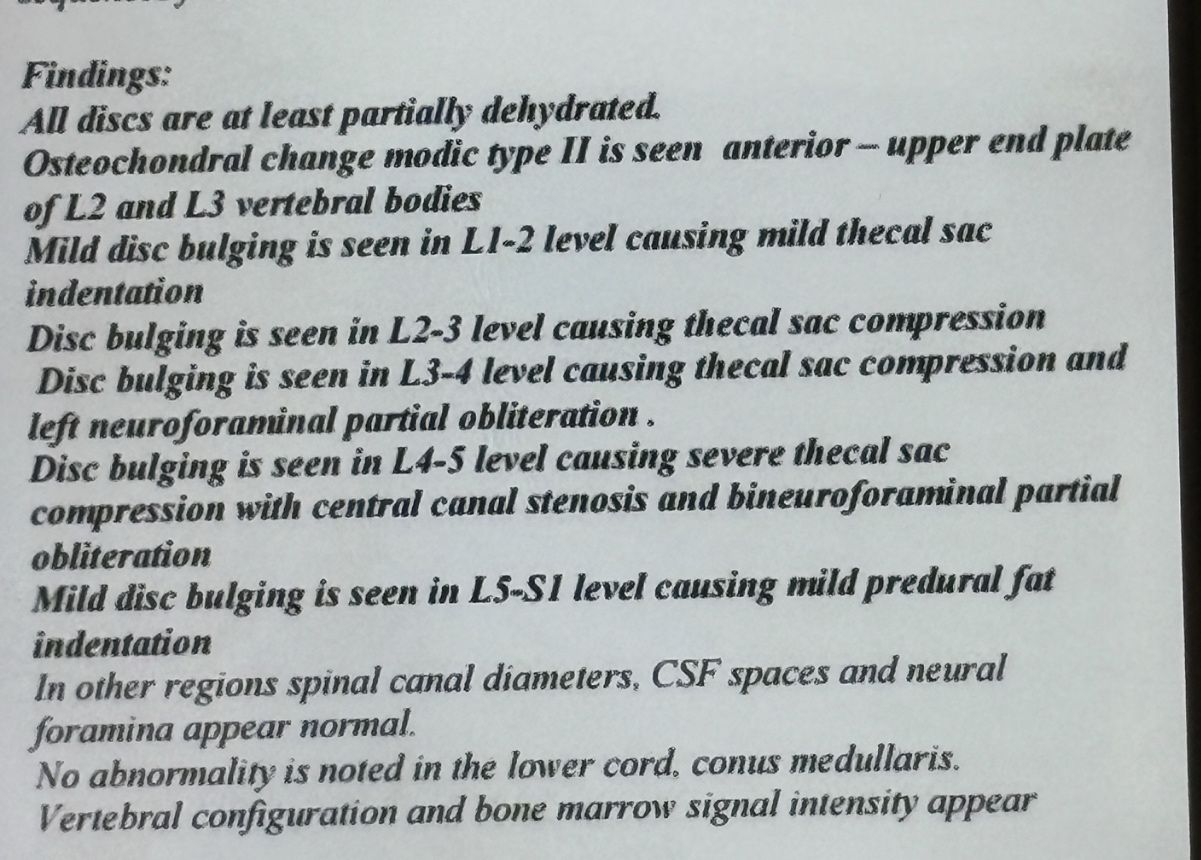
32 years female patient presented to my office one year ago with moderate cervical pain and R. Arm pain ,mild LBP with no radicular pain. Her mri in C/s had few bulges and few segmentsl dysfunctions
Her lumbar mri showed Contained R. Para. L5-S1 extrusion
She got treatment just for her neck and exercises for her low back. Few months later had lumbar disc surgery
Few days ago on may on june 08/2025, presented with severe LBP and no radicular pain
I have post her lumbar MRI before and after surgery. I consulted with a neurosurgeon at our clinic and he said doesn’t need another surgery because doesn’t have radicular pain or neurological deficits
For her pain i have started to do mild decompression by Cox and DTS and acupuncture, no adjustment whatsoever.
Please mention what differences you see before and after surgery
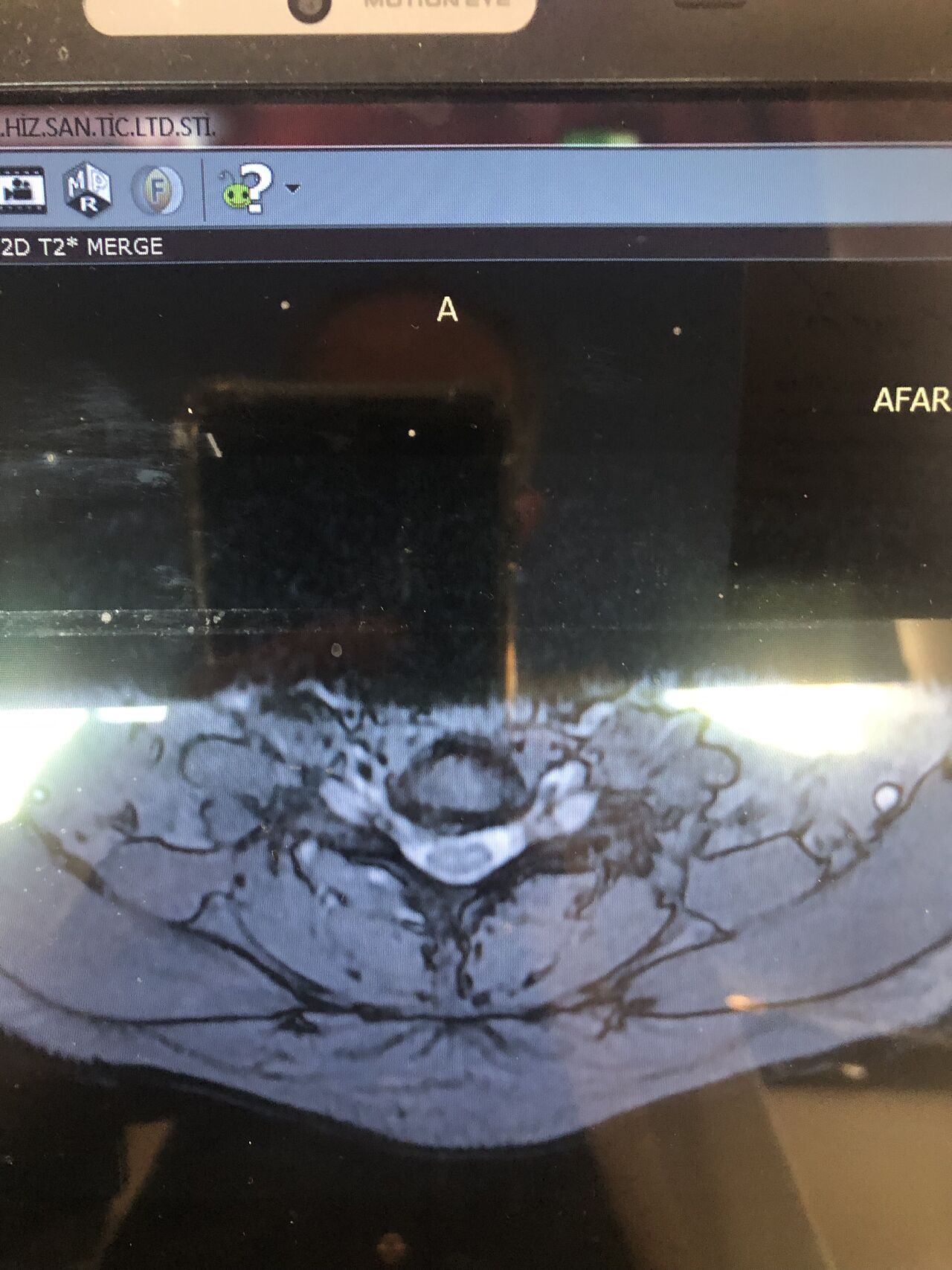
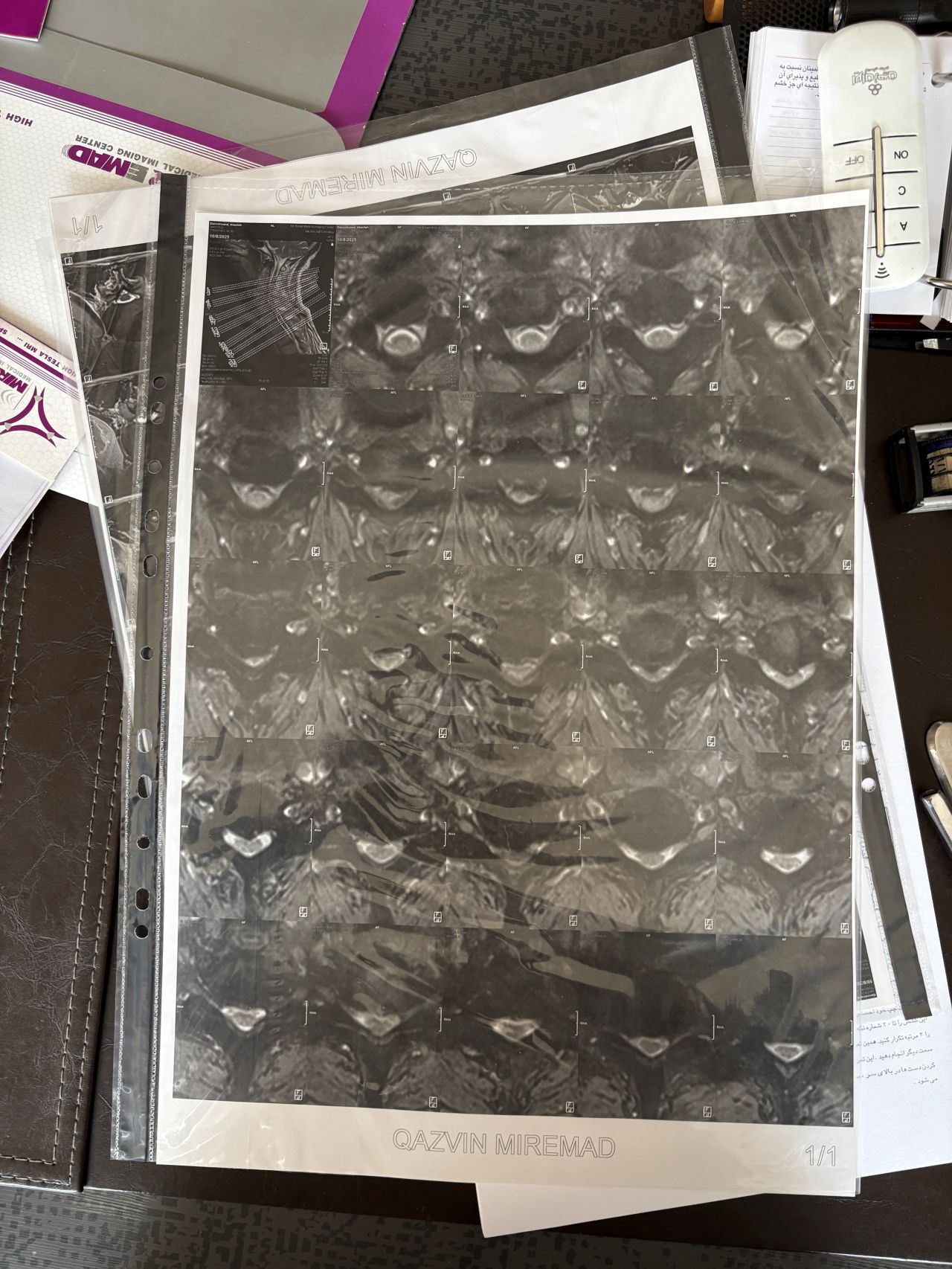
Case 7
60 years old female patient presented to my clinic today,
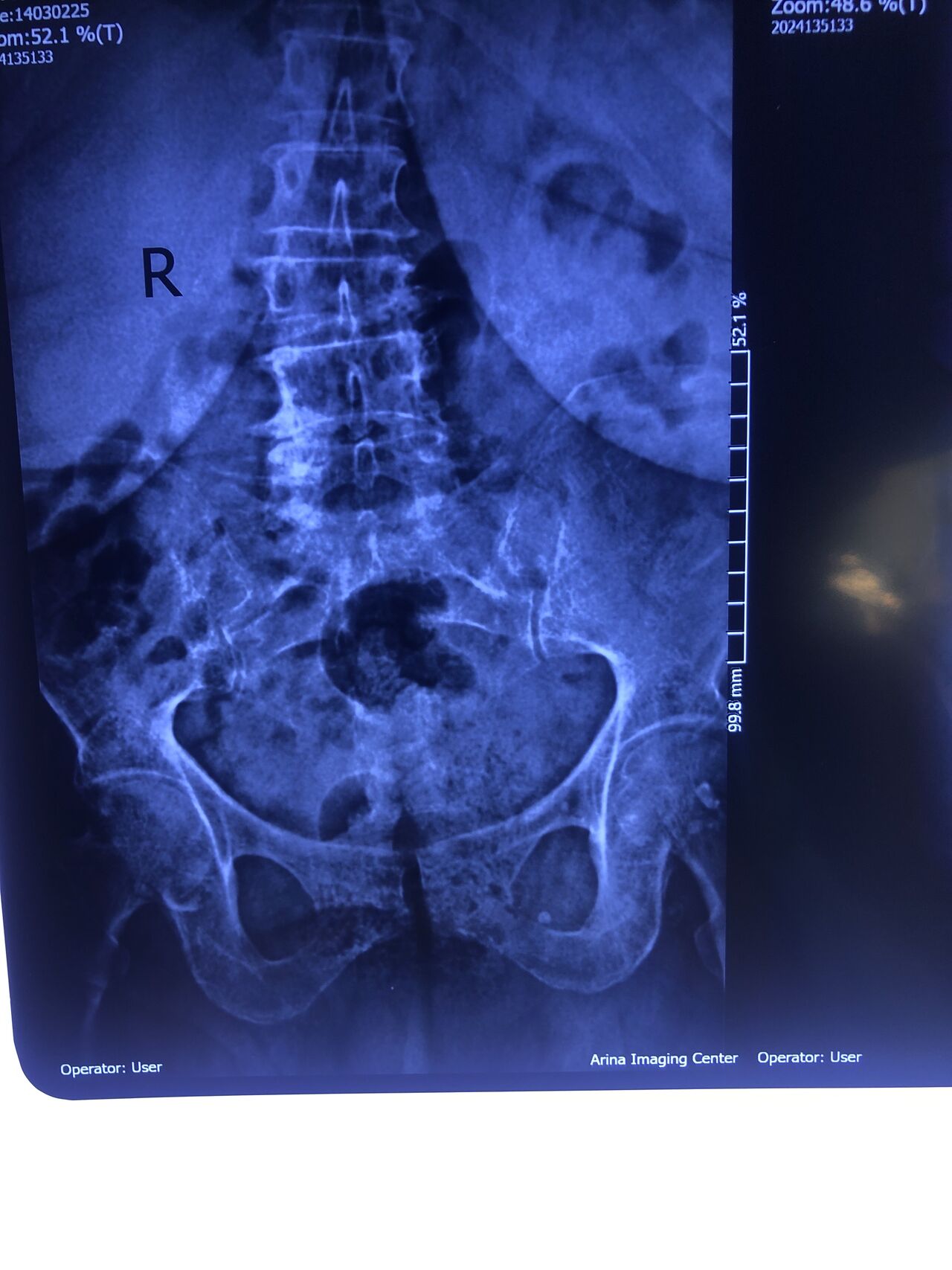
May 31/2025 with R. Chronic pelvic pain which gets aggravated by walking. Her lower extremity motors all were fine
She has had chronic neck pain as well with radiation to R Upper extremity
I would like to show especially to new grads some information and improve their x ray and mri readings
Would be so great to hear from chiropractic doctors or any other specialist other findings we may have missed
Findings:
L4-L5 level:
sever L4-5 canal stenosis mainly due to FL hypertrophy?
CSF block. Mild L3 retrolisthesis, facets hypertrophy bilateraly causing L and R IVF stenosis, disc hyperbule
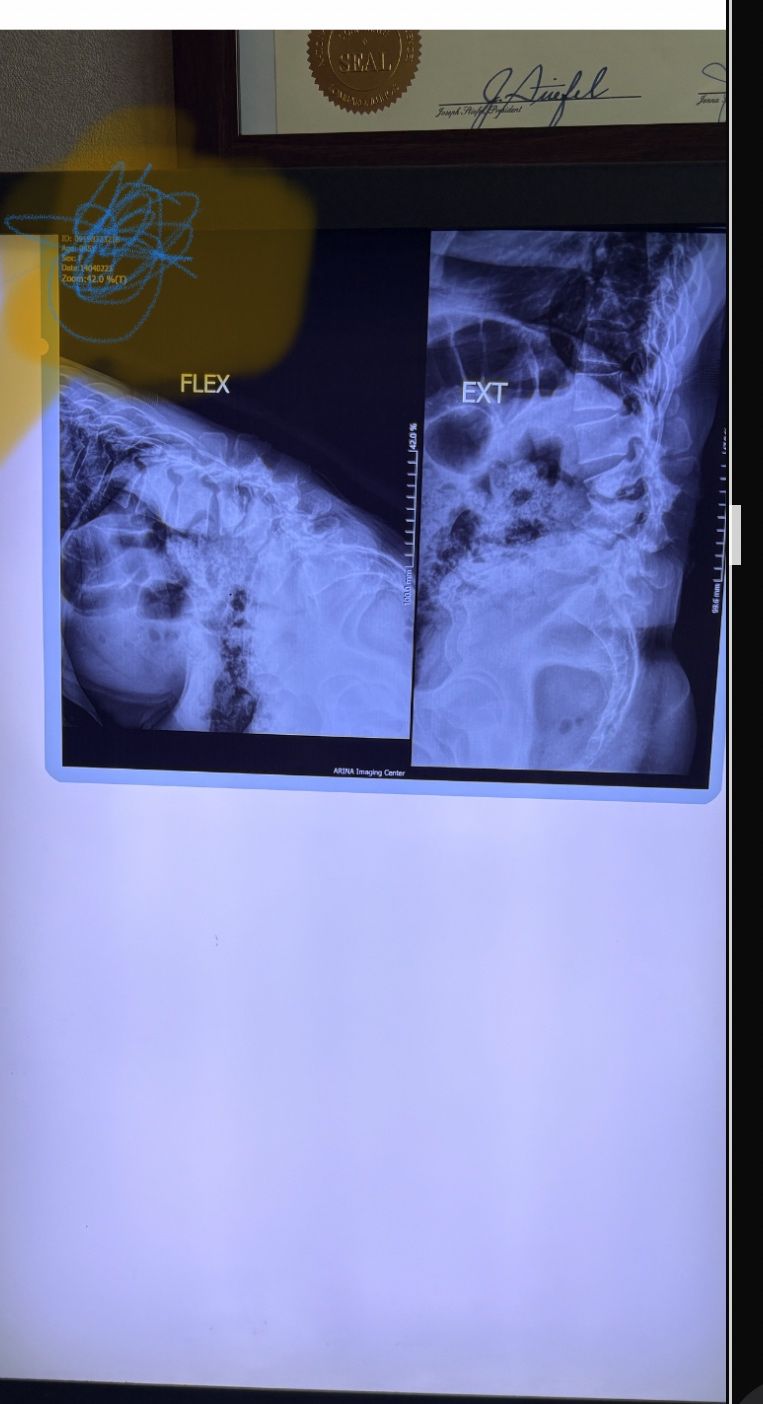
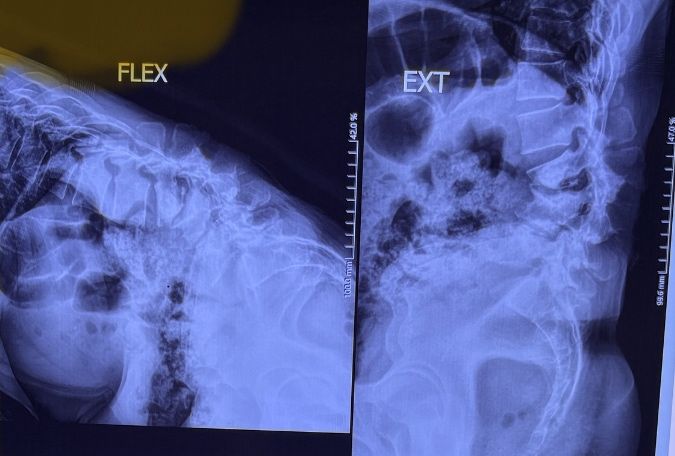
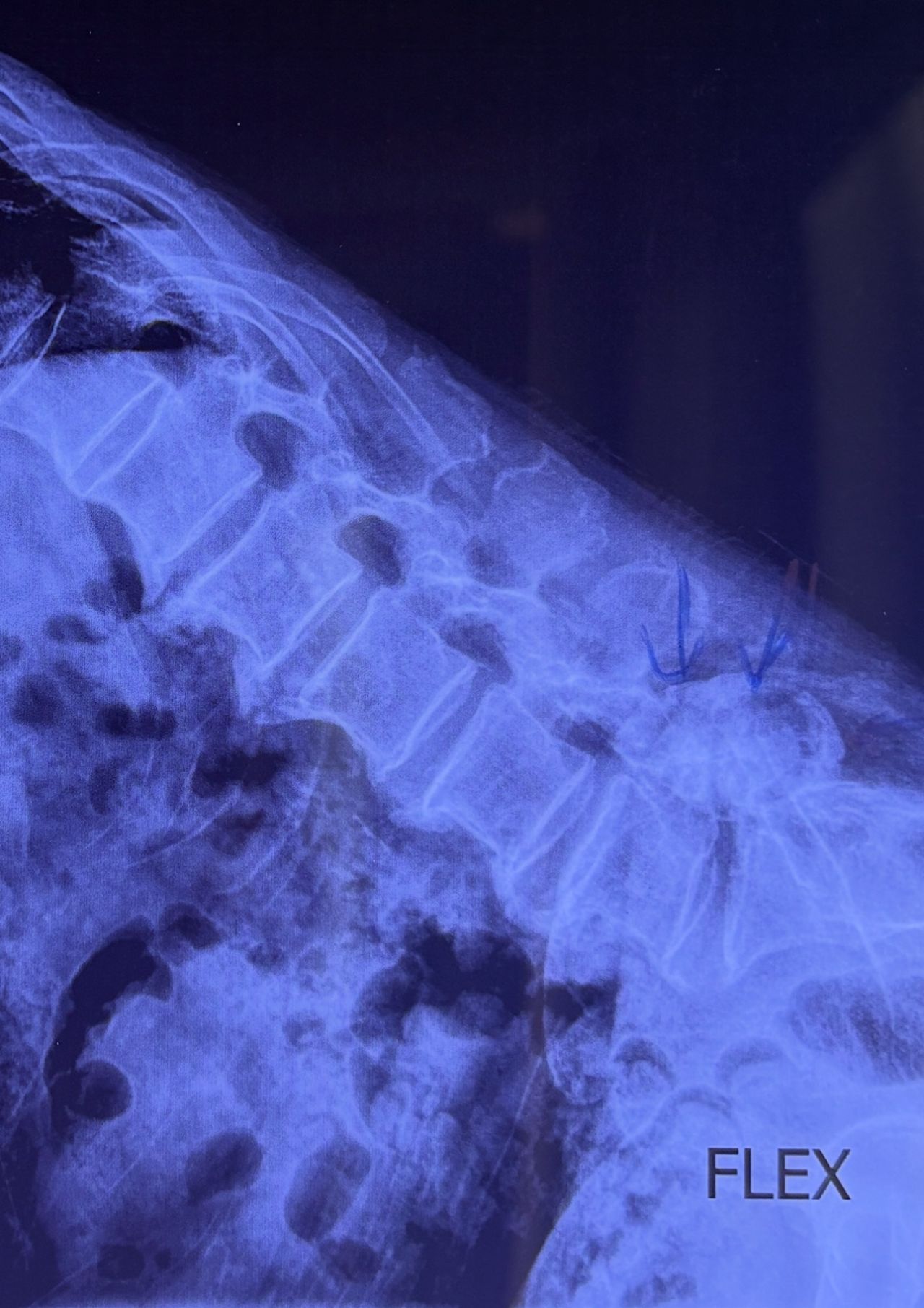
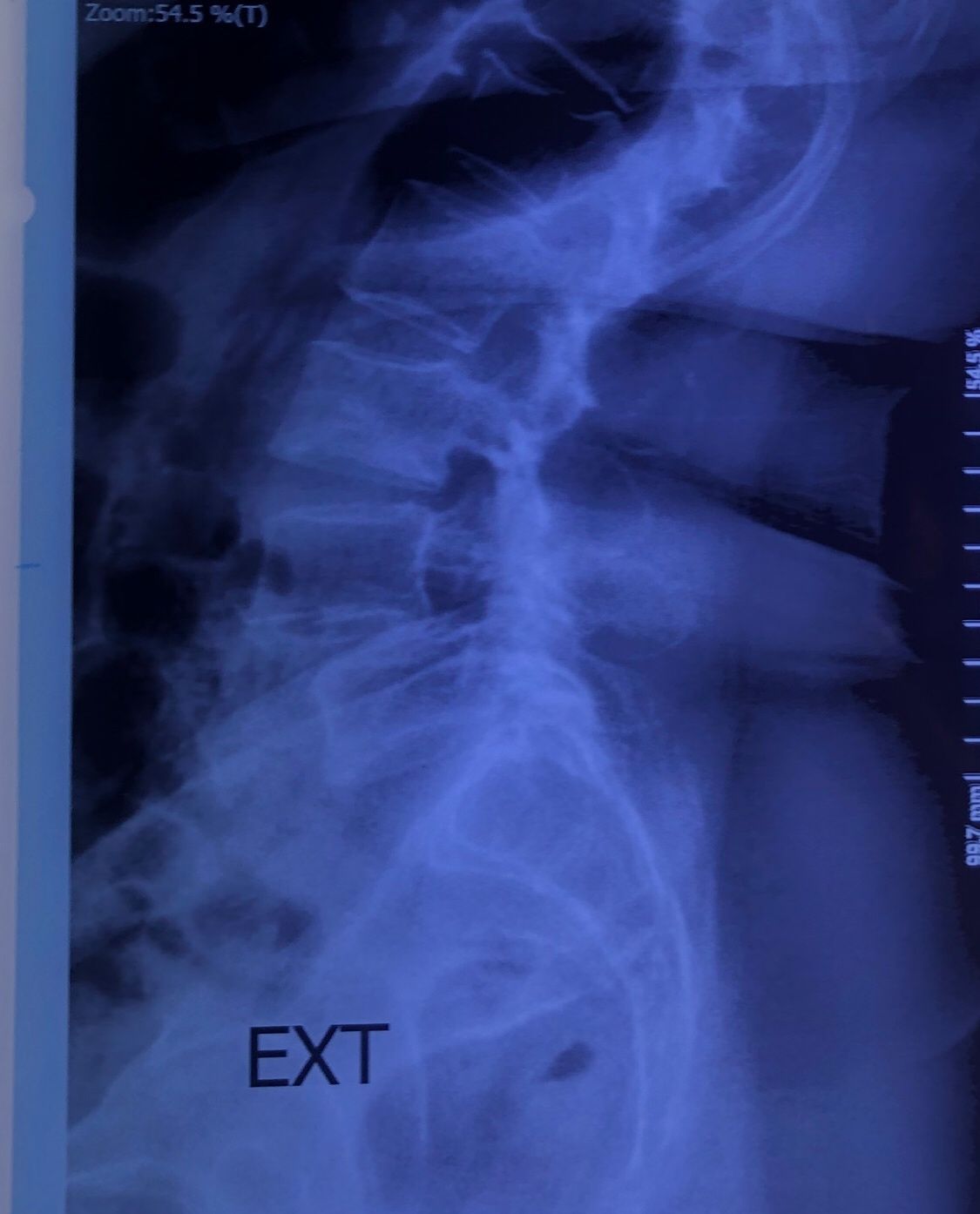
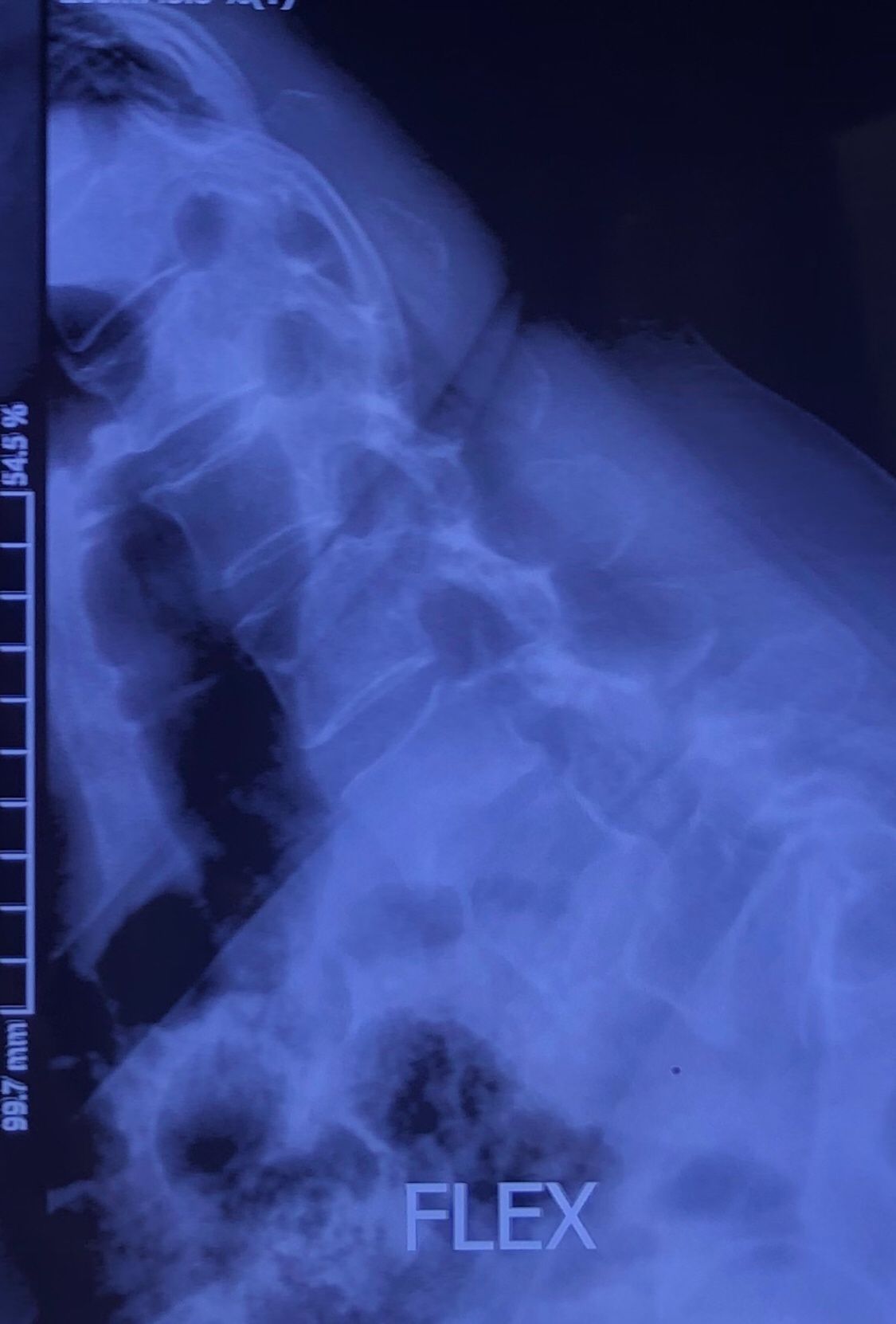
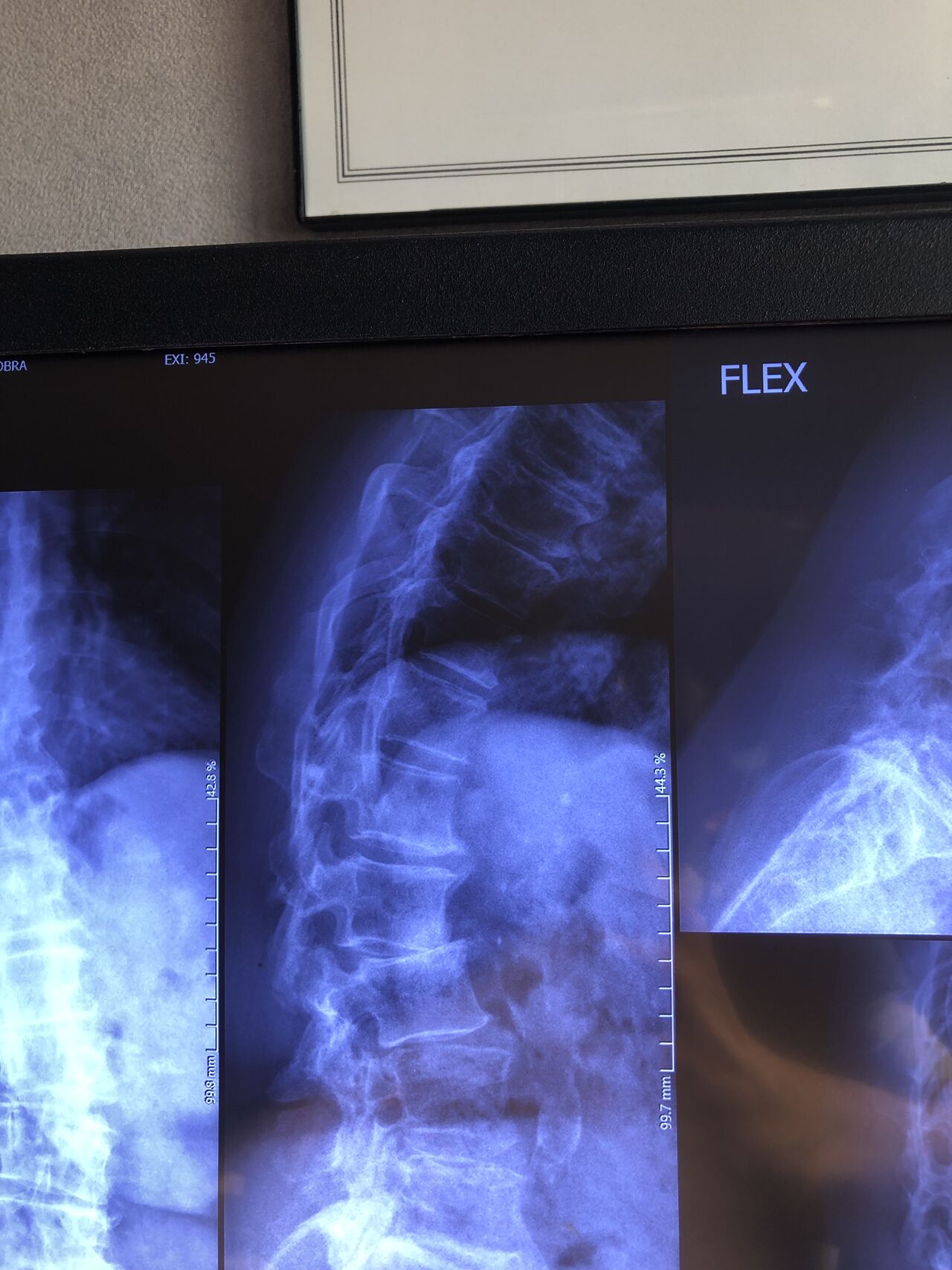
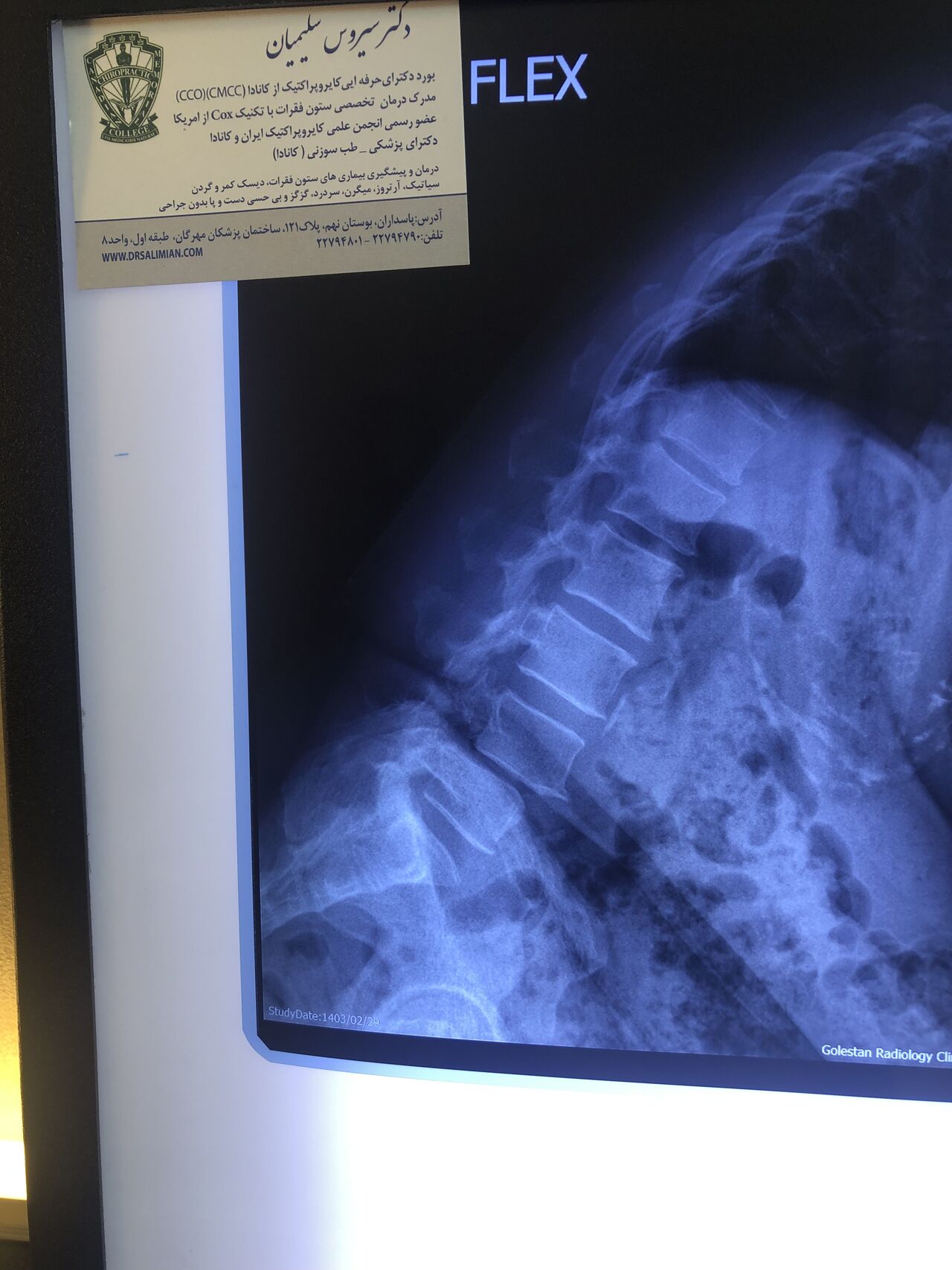
Since I’ve noticed instability in some segments I asked for dynamic L/S x ray:we see mild L4 ant listens due to DjD/DDD. There is not any pars defect.
In cervical mri I marked some findings plus their reports
I will give her treatment via Cox chiropractic flex dis and axial decompression. I would use DTS decompression
Since there is a few mild to moderate DjDs/ DDs in her lower back I won’t use lumbar adjustment on her
Case 8
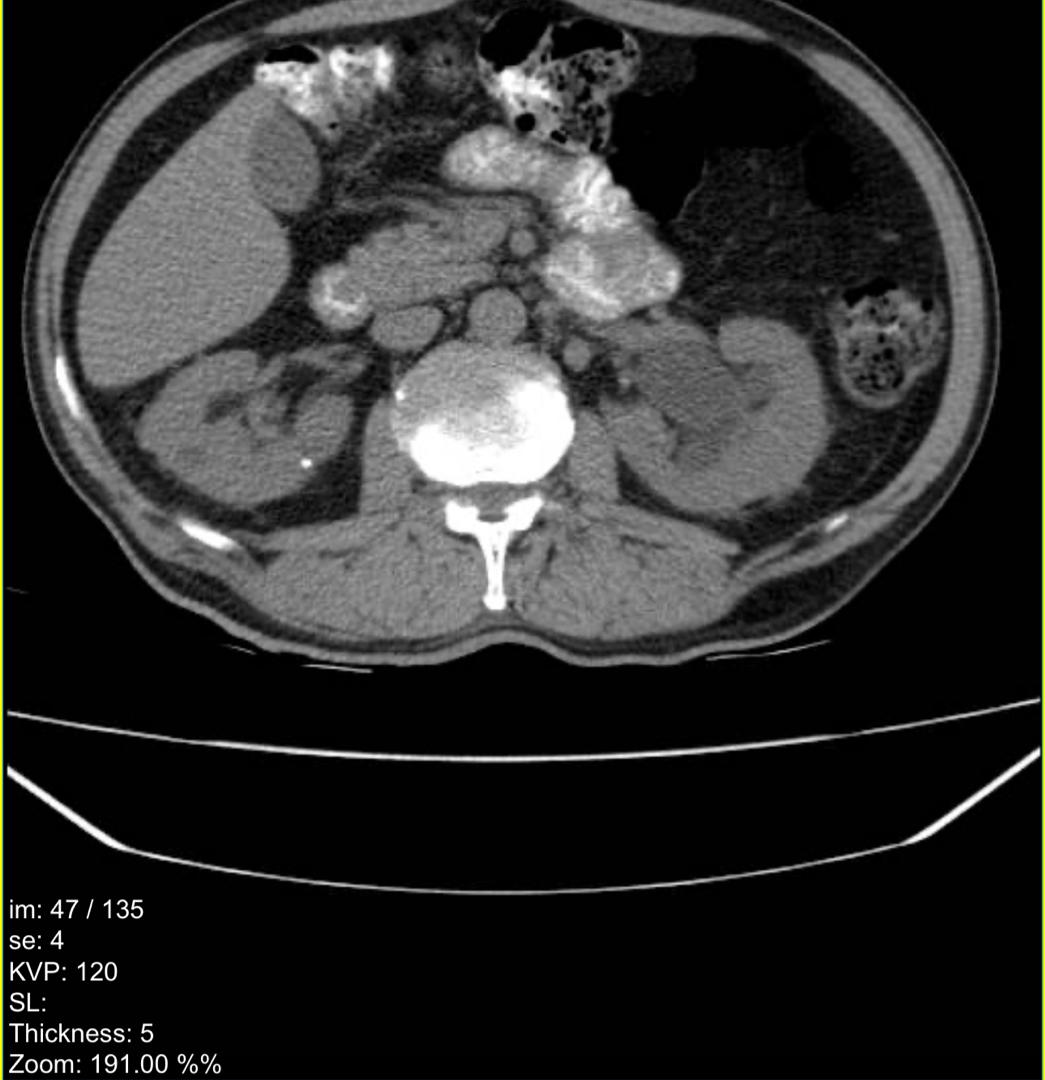
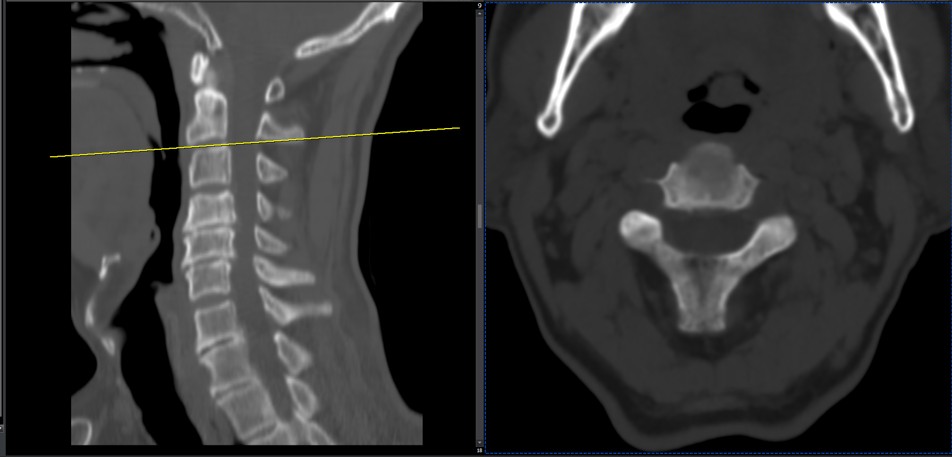
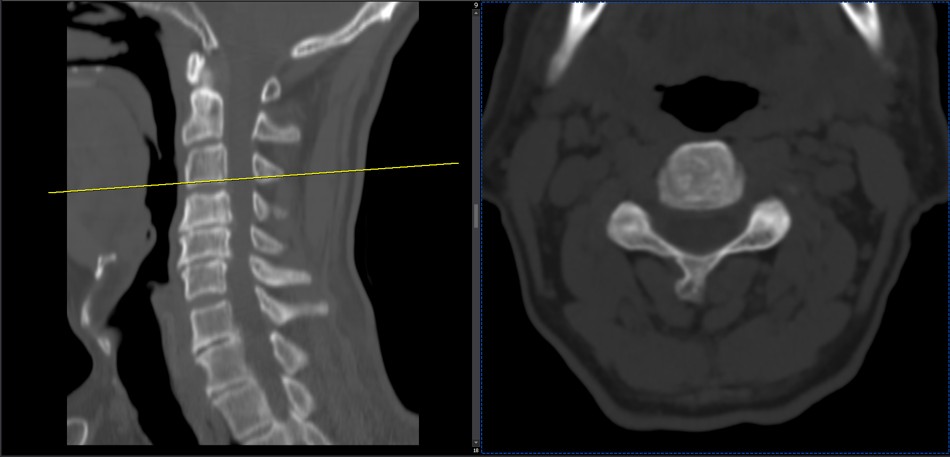
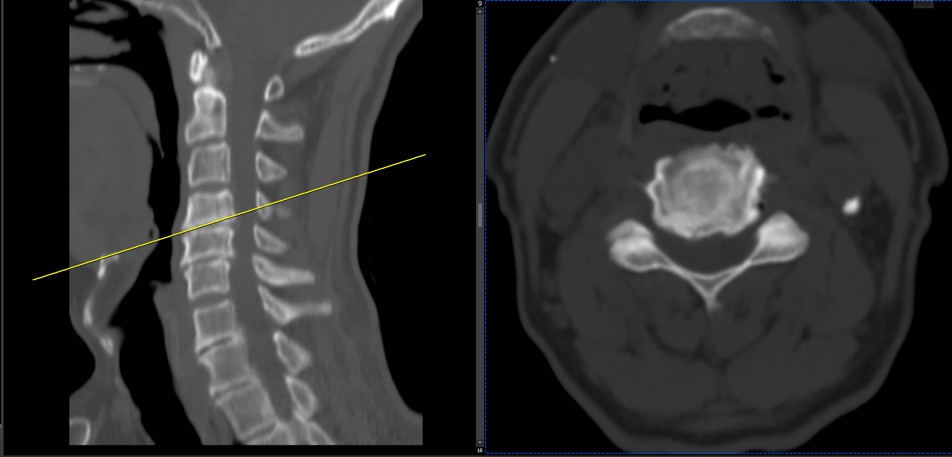
Few weeks ago I posted a case with an old TB spondylitis and listhesis with old fractures and severe canal stenosis (in her lower lumbar). A neurosurgeon who works with us at my clinic saw her in the second session
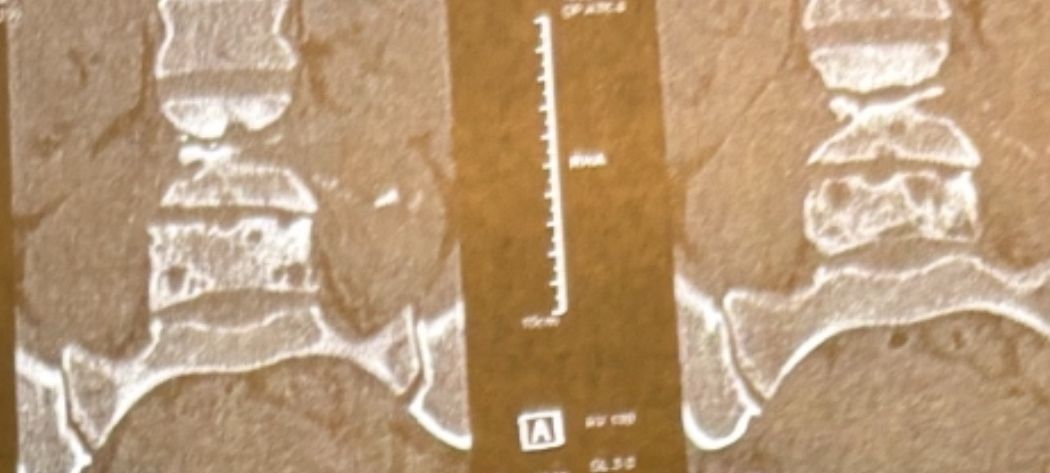
I attached her CT scan. Her PPD which was positive 2 months ago now it’s less than 3 mm. Since this patient has just low back pain and no radicular pain and can walk easily our neurosurgeon suggested no surgery and we emphasized that she has to complete her medication and be under her infectious diseases specialist
And if other signs and symptoms develops have to see surgeon again
Case 9
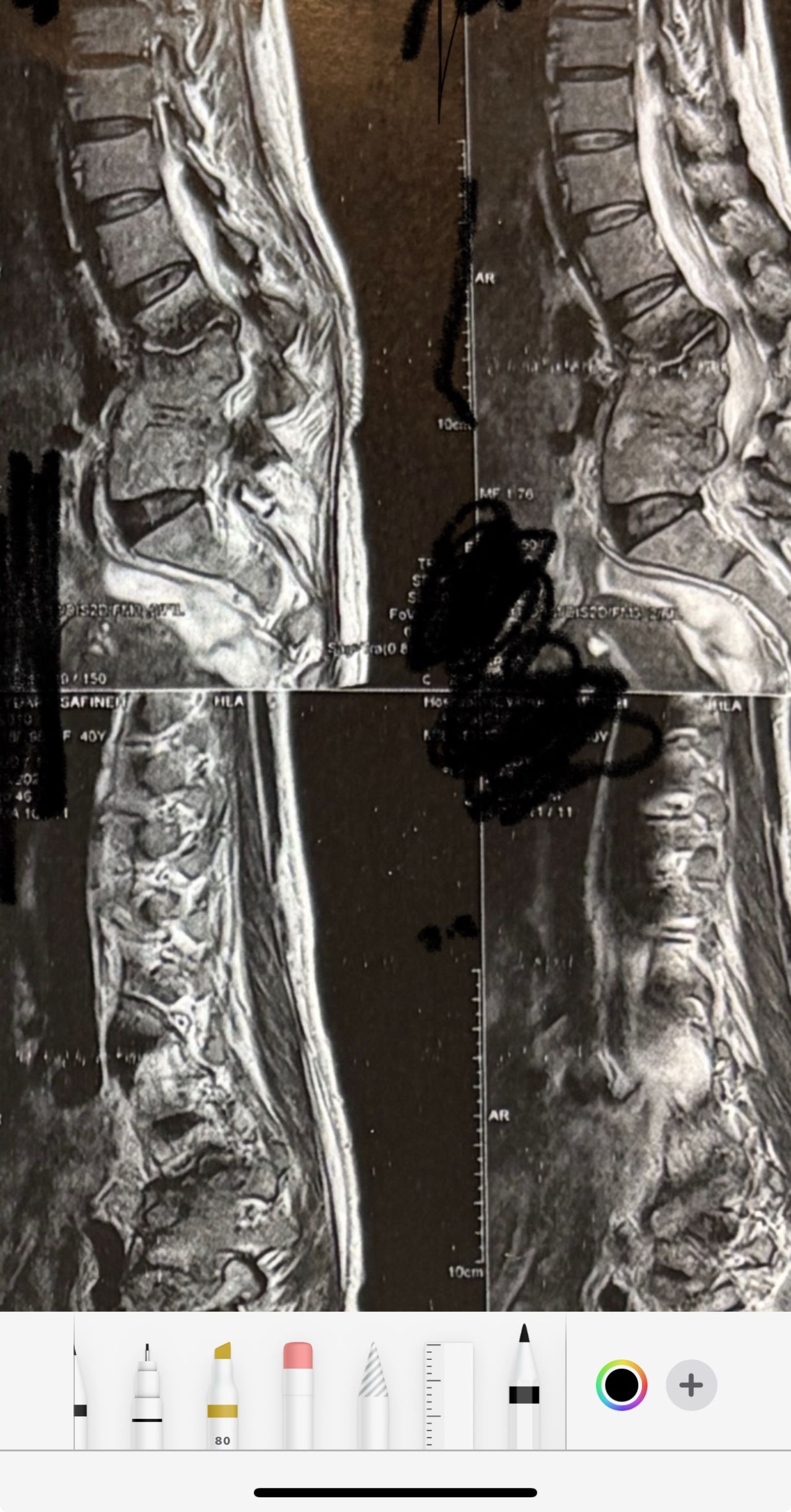
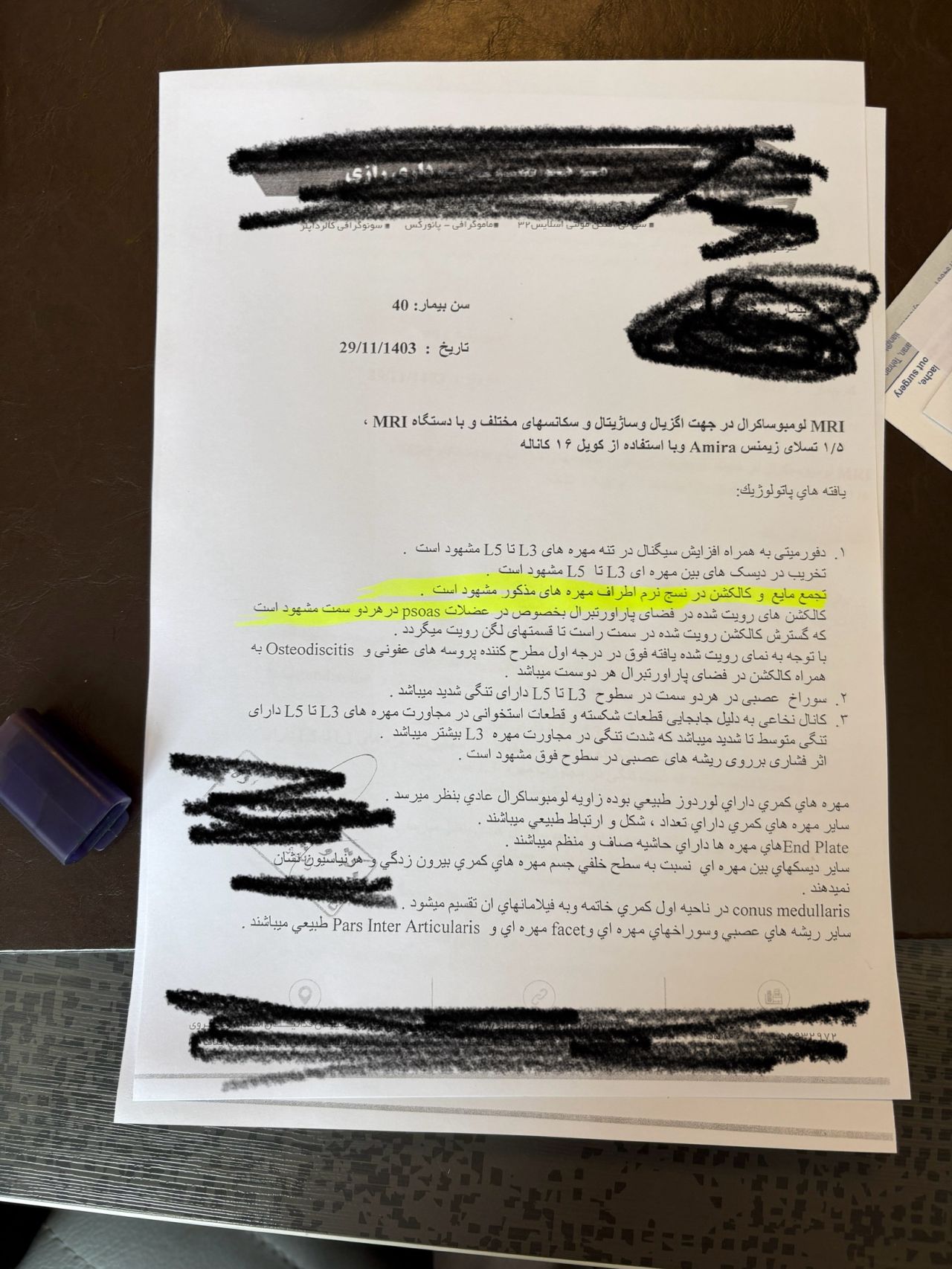
42 years old female presented to my clinic yesterday on May15/2025 with chronic Low back for 2 yrs. She is from afghanestan and arrived to tehran 3 month ago. Visited pain specialist 3 months ago who just did PPD test and gave her Anti TB medication. In examination just had severe focal khyphosis from L3 to L5 without any tenderness. Her mri was done 2 months ago. Report is in Farsi and mentions of paraspinal puss/ fluid collection esp in psoas muscles, with extension of fluid collection to R pelvic region. Had 2 site of severe canal stenosis due to previous fractures of L3,4,5 and movement of fractured bones to the canal with complete distractions of those levels discs with fusion of L3 to L5
I ordered C T scan of lumbar and pelvic MRI / chest x r and reffered her to neurosurgon and infectious disease specialist to get full assessment and possible hospitalized for biopsy and surgery
As you know doctors of chiropractic would never. give treatment to patients with spinal Discitis/ osteomyelitis/ metastasis/ fracture( absolute chiropractic contraindications for treatment)
Case 10
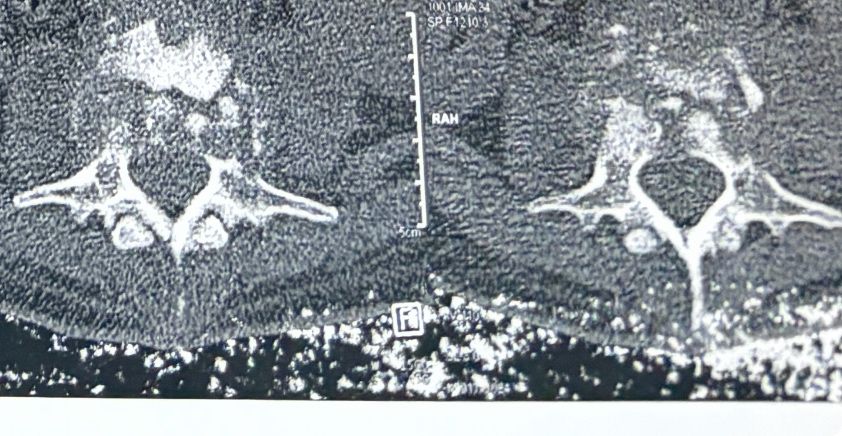
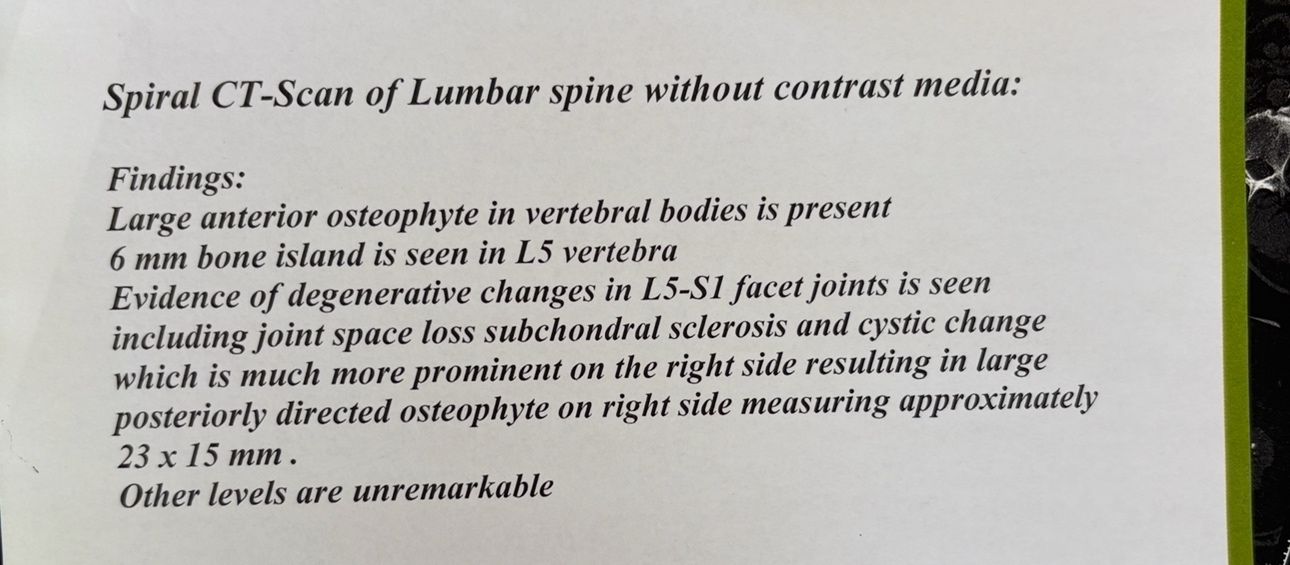
62 years old male presented to our clinic due to legs heaveness/tireddness in walking 2 weeks ago. 9 months ago had cervical disc herniation surgery. Had no LBP, no radicular pain. All neuro exam were normal. In his mri and dynamic scan there was a big osseous mass behind L5and S1. In his x. Ray report just was mantioned DJD
Radiologist missed that large osseous mass. Radiologist missed that bony post mass in x ray and mri. We ordered CT scan.
Case 11
40 yrs old female patient presented to my office on Feb 08/2025 with severe R post shoulder pain along C6-5 dermatome since 3 weeks ago.Had physiotherapy, didn’t help. Her mri 3 months ago and the new one few days ago were the same and showed R. para R. IVF C5-6 moderate size protrusion. Her exam was normal. After 5-6 sessions of treatment she has got 60 percent improvement P
Case 12
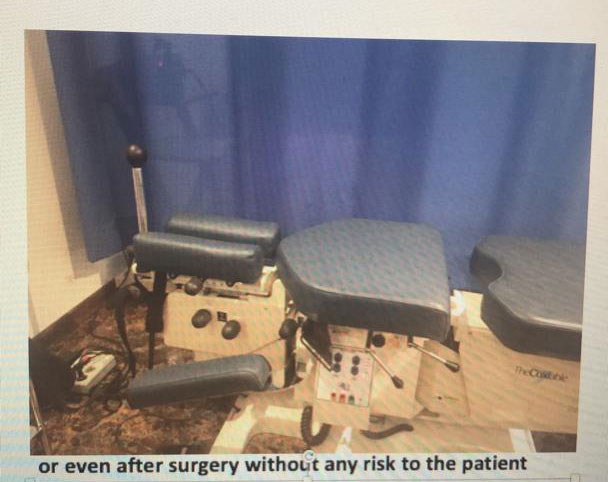
Cox decompression flexion axial distraction treatment on cox chiropractic spinal table
Chiropractic doctor should take cox technic courses for a few weeks and pass written and practical exame to get certified in this technic and have to buy the table from USA( US made)
For treatment of spinal disc herniations and stenosis
Case 13
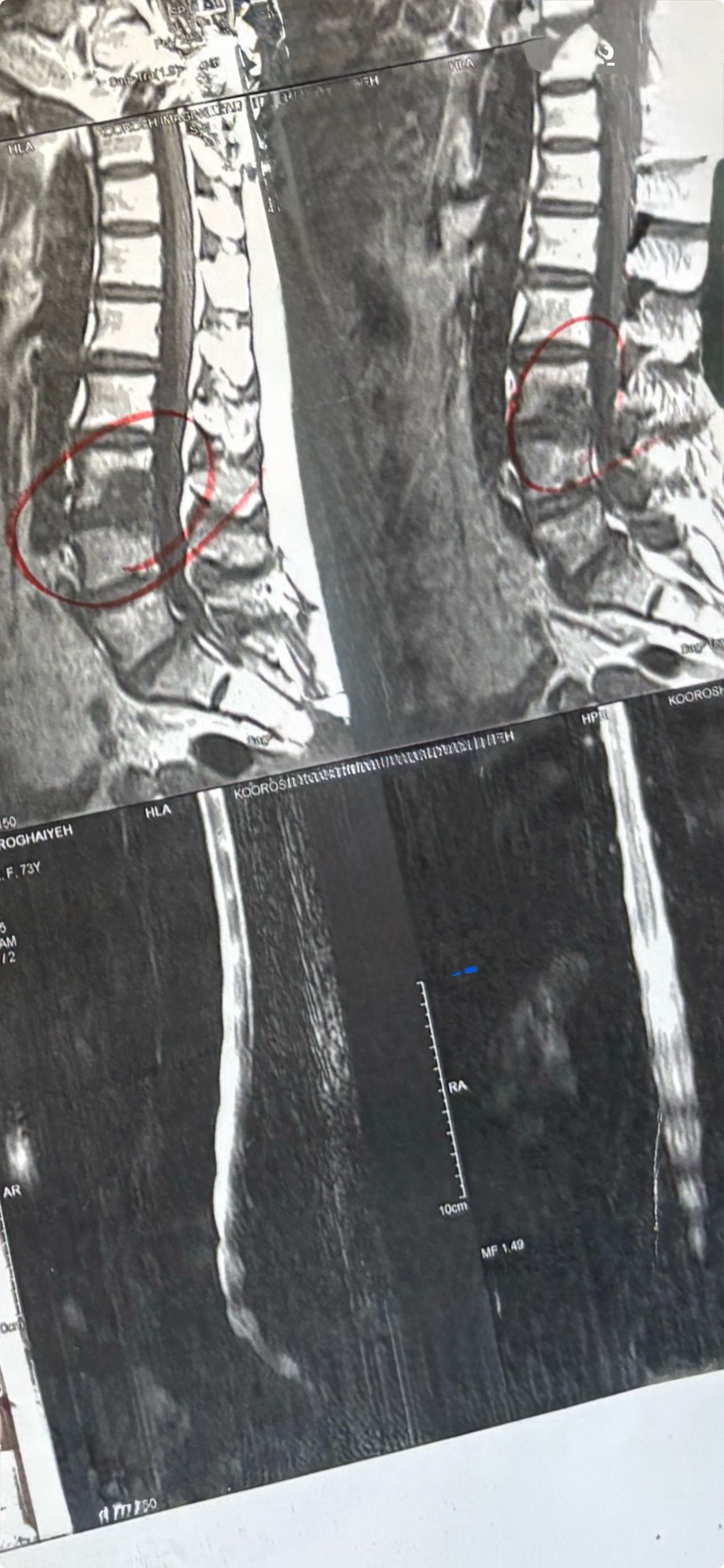
72 years old female patient was my own patient since 15 years ago due to LBP who had severe spinal osteoporosis ( T score -3.4)with T12-T11 and L1-L2 protrusin, and had chiropractic care from me via flex/distraction and decompression, had no adjustment due osteoporosis for several years + has had reoccurrences several times and last time i visted her was6 years ago with the same disc herniations .
Didn’t show up till few days ago on Jan/2025).
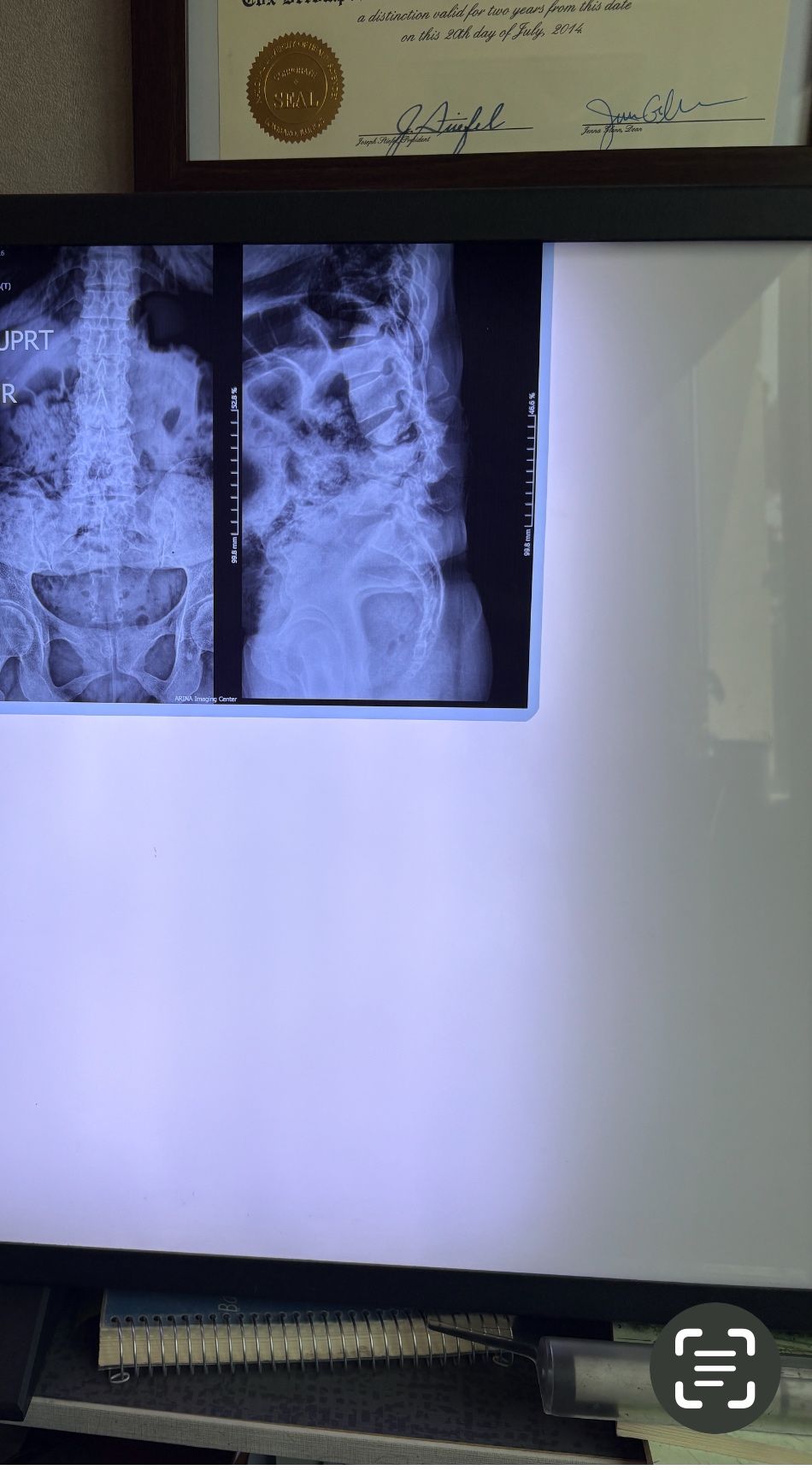
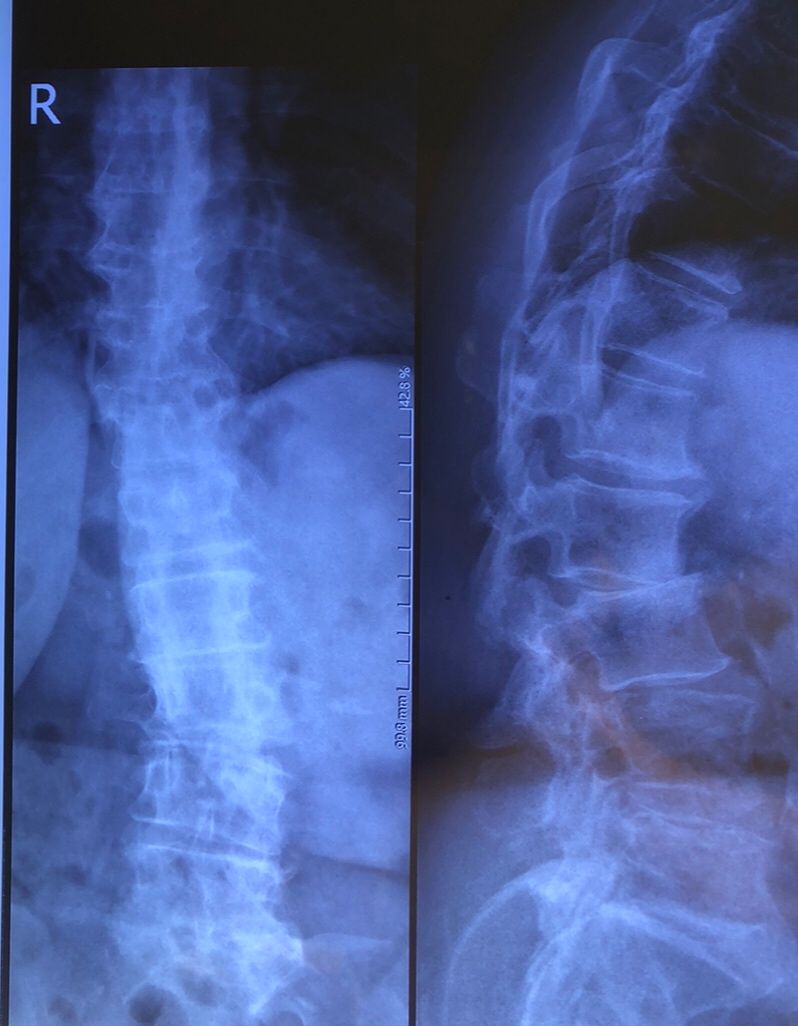
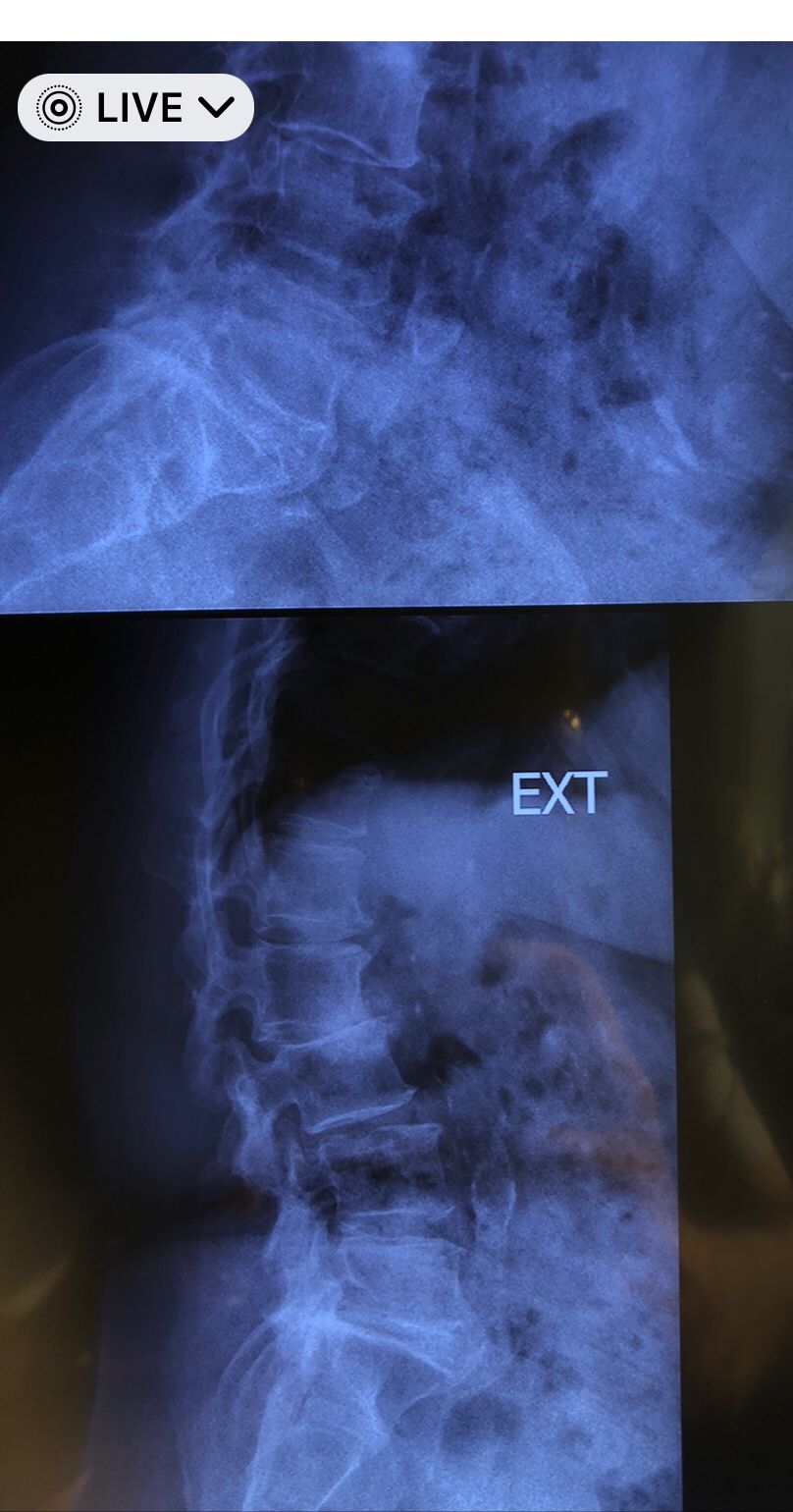
This time presented to my cl with LBP mainly during sleep at night. Just brought me her mri. According to her mri I ordered dynamic L/S X. R.
I didn’t accept her to give treatment. I referred her to her surgeon. What are your findings in her mri and X. Rays?
Is ant listhesis of L4 unstable or stable?
From several compression fractures we see which of is acute/ subacute and which ones are chronic fx?
Case 14
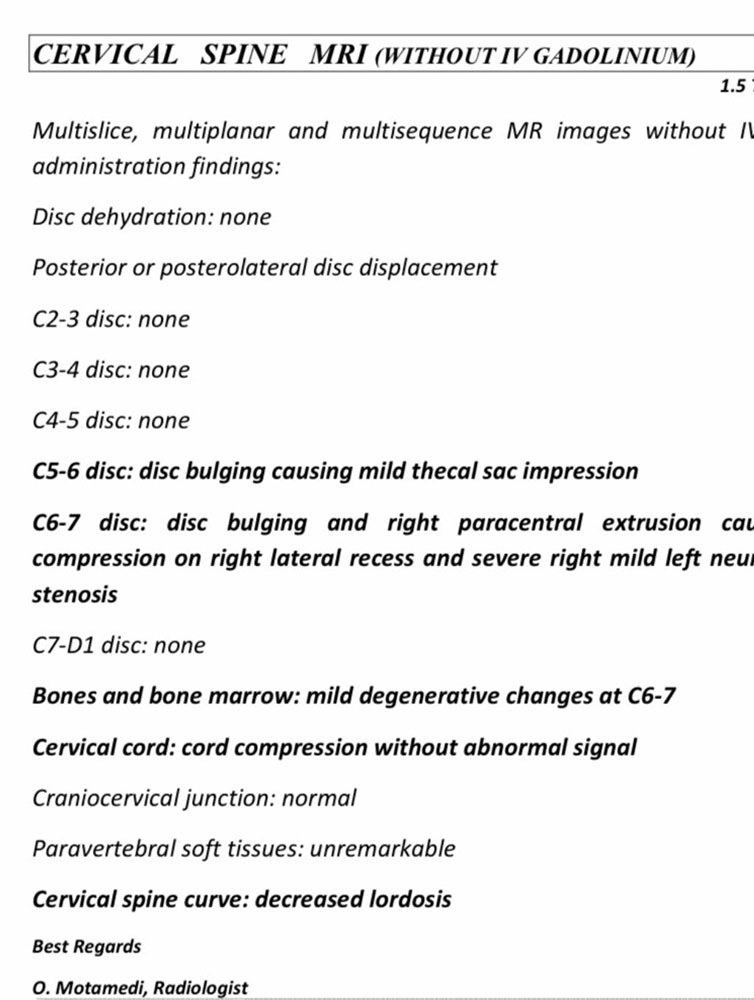
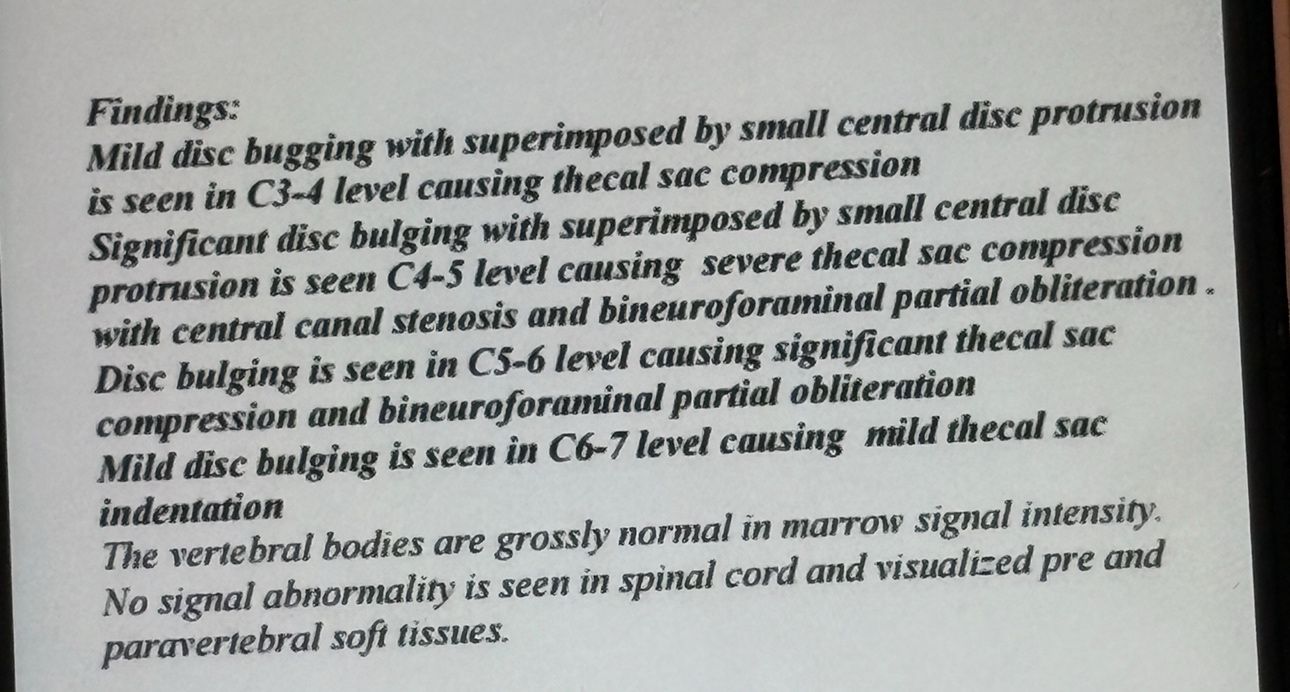
53 yrs old femal presented to my clinic on Jan/2025 with neck pain which was started 40 days ago. In the last 5 days pain was increased without any radicular pain. Had done mri and saw an experienced chiropractor and got 5 sessions of cervical adjustment/SMT which was so helpful in decreasing her pain. I repeated her cervical mri and did EMG/NCV( just had mild c5,c6 radiculopathy). In examination had no UMN signs. I have posted her mri before and after adjustments by another chiropractor.
I didn’t accept her for treatment.
Was cervical SMT a wise decision to treat her cerical disc Extrusion? What could be her complications after adjustment(even though her pain was reduced a lot after those adjustments?)
If you had visited this patient first, what would be your plan of management for her?
Case 15
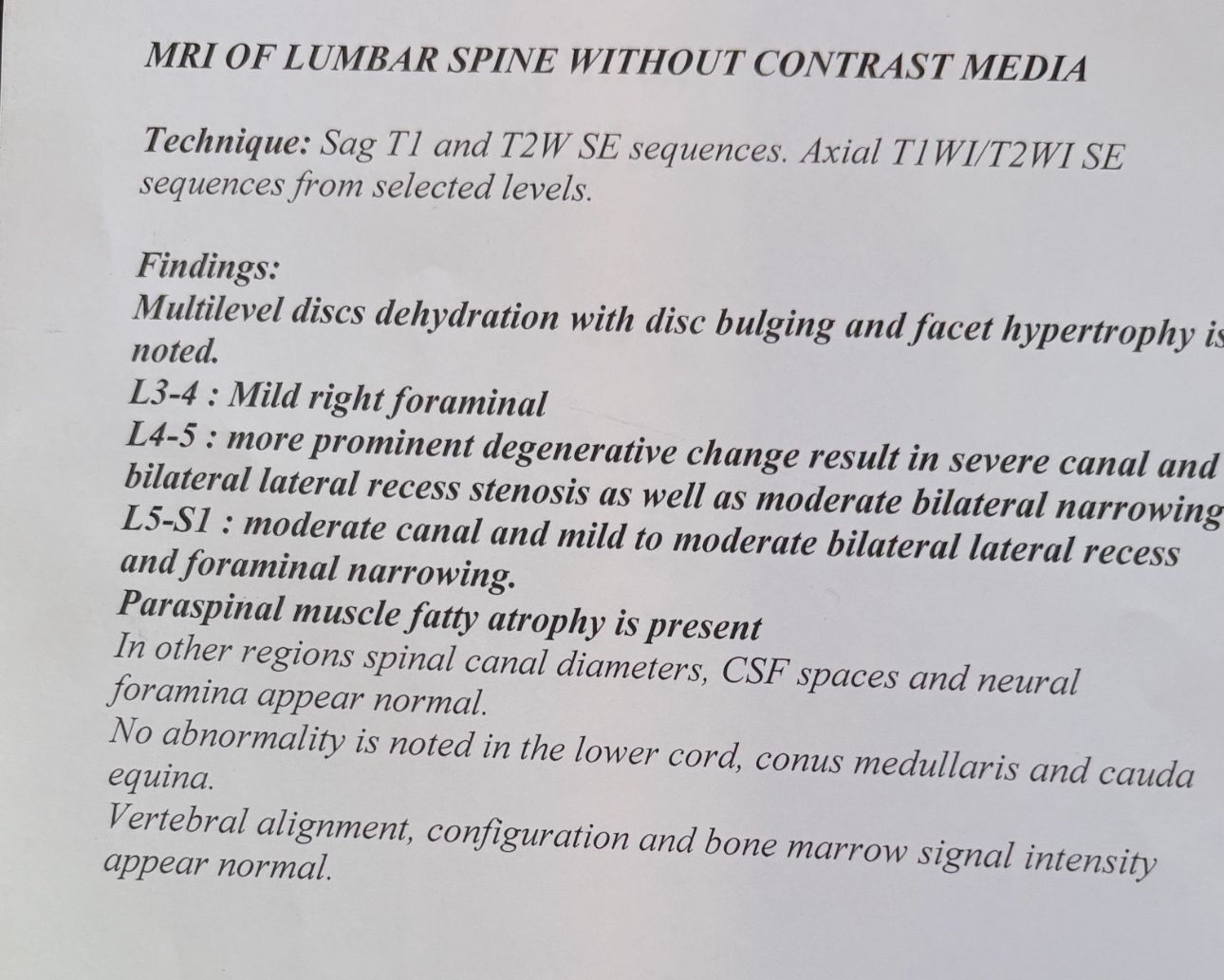
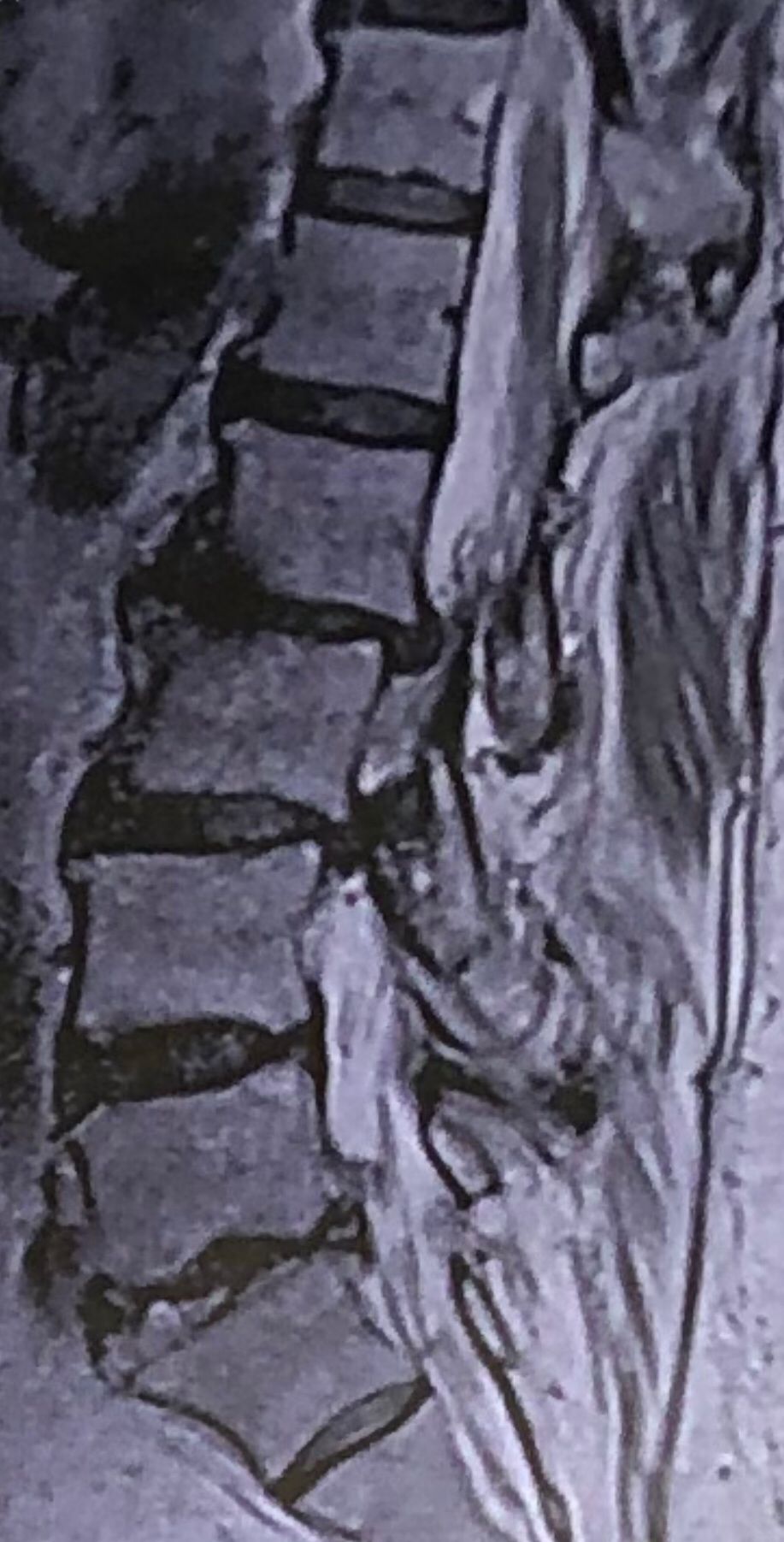
70 yrs old female presented to my clinic today (Oct 06/2024)due to severe LBP with both legs pain for several years.
7 years ago came to my clinic with L leg radicular pain and I referred her to a neurosurgeon. Patient underwent full laminectomy from L1 to S1. Few months after surgery her LBP and legs pain were started and hasn’t improved since then. Now walking aggravates the pain and forces her to bend forward. Patient had mri from 6 months ago. Her mri 7 years ago was similar to the recent mri, just laminectomy and soft tissue collection has been added. In neurological examination p.tvdid not have any neurological deficits. I ordered lower limbs emg/ncv, dynamic lumbar spine X.ray. As a chiropractic Doctor what would be your plan of management for this patient?
Case 16
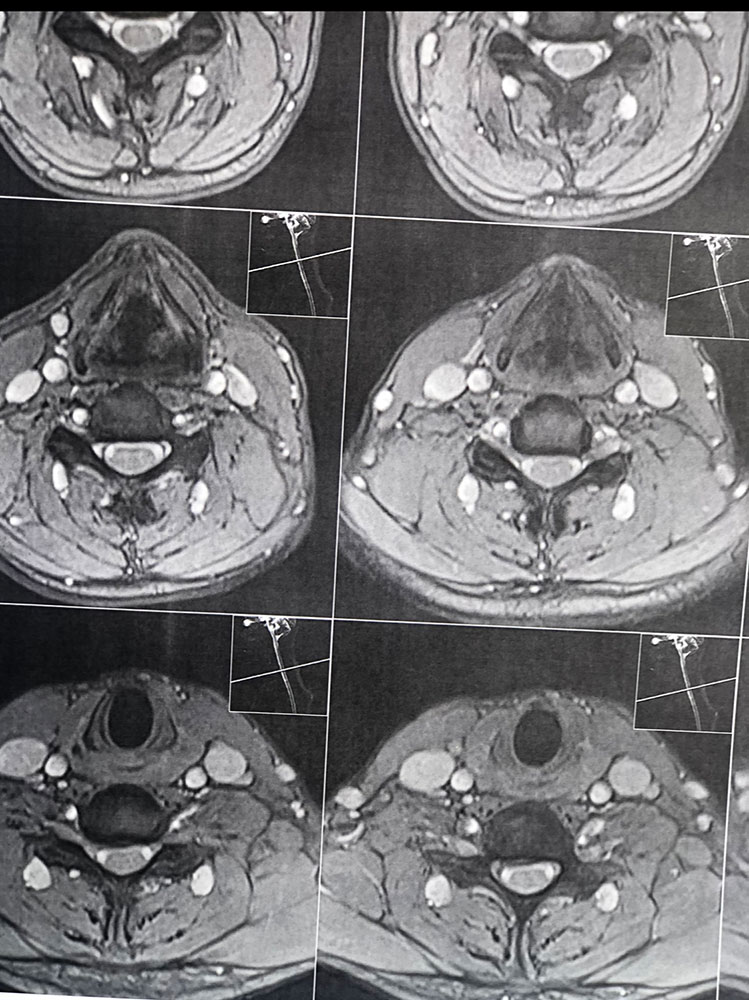
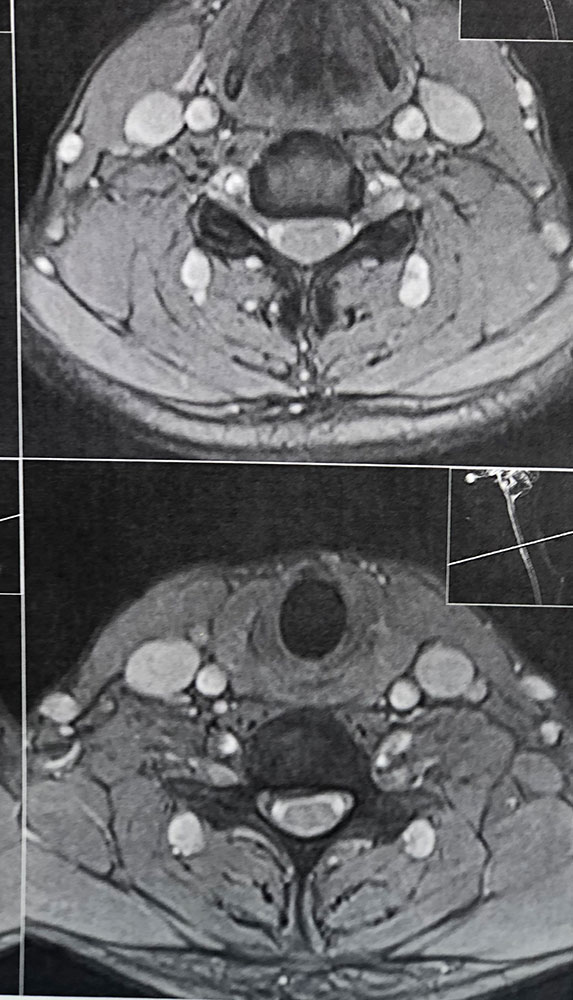
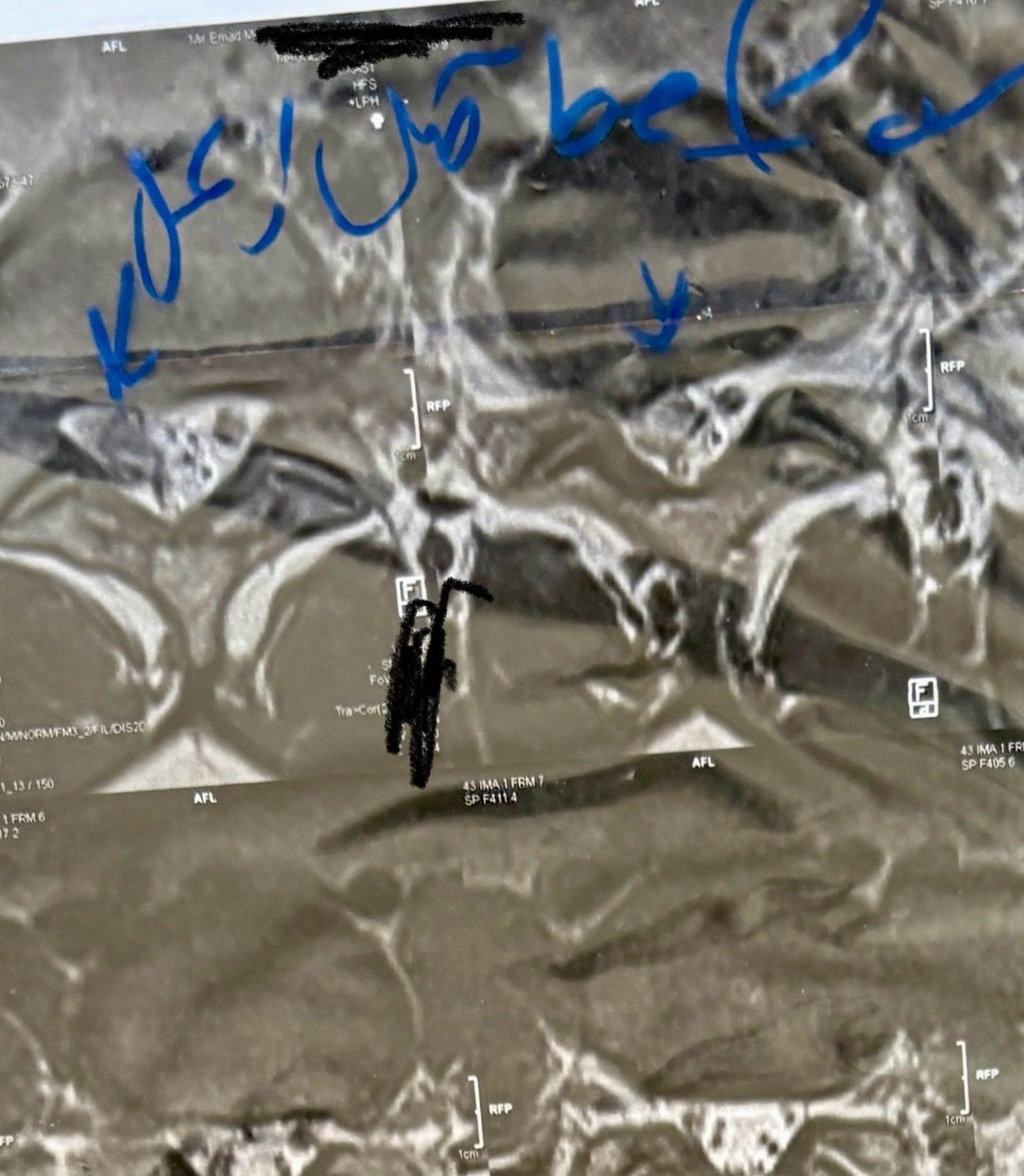
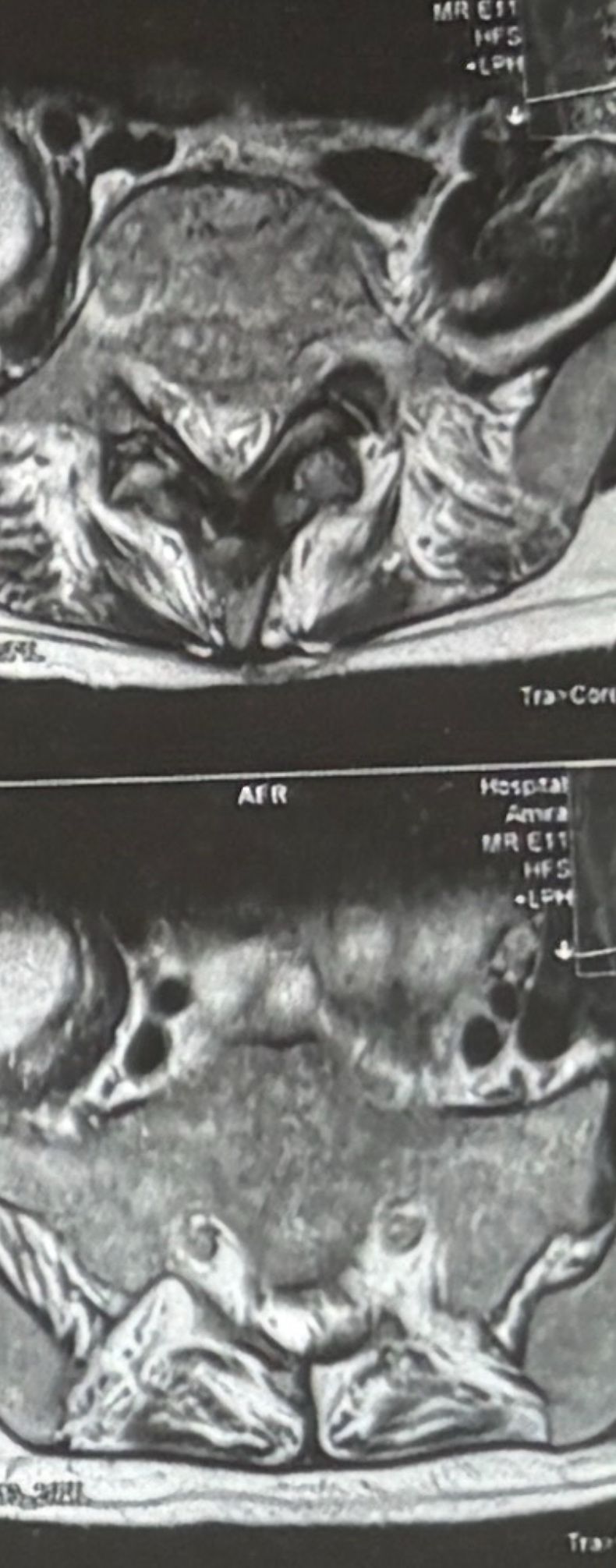
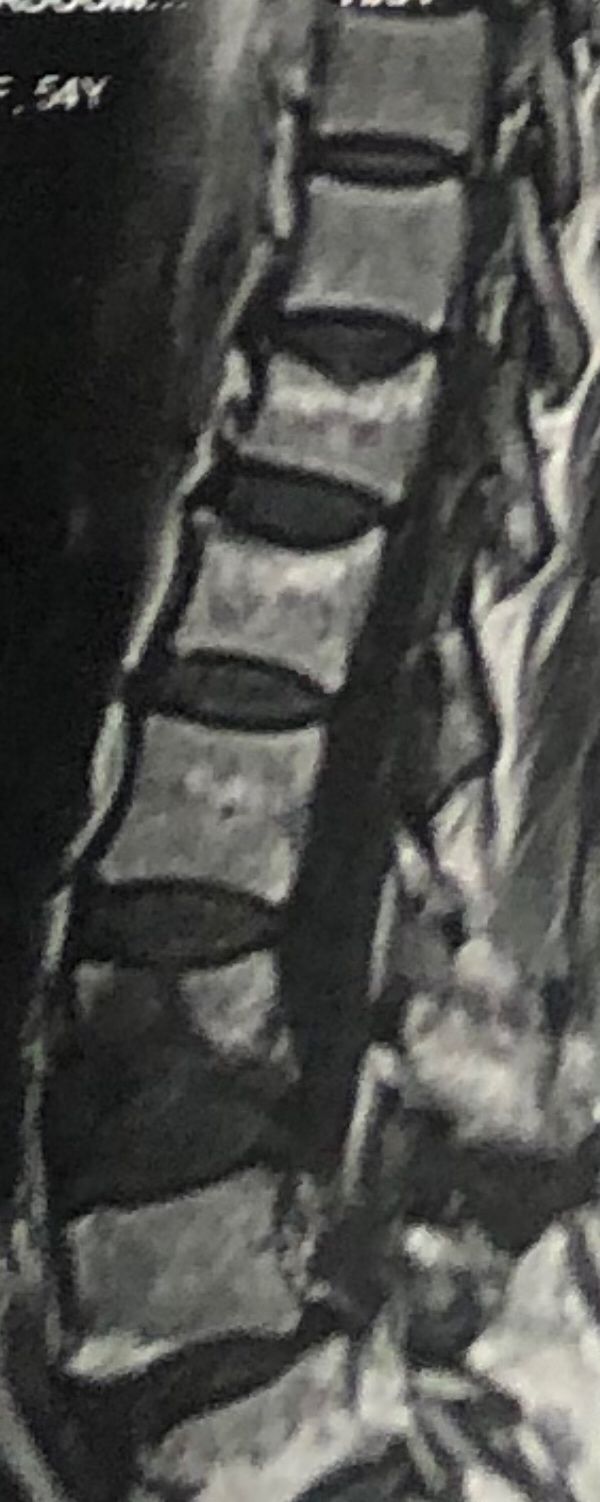
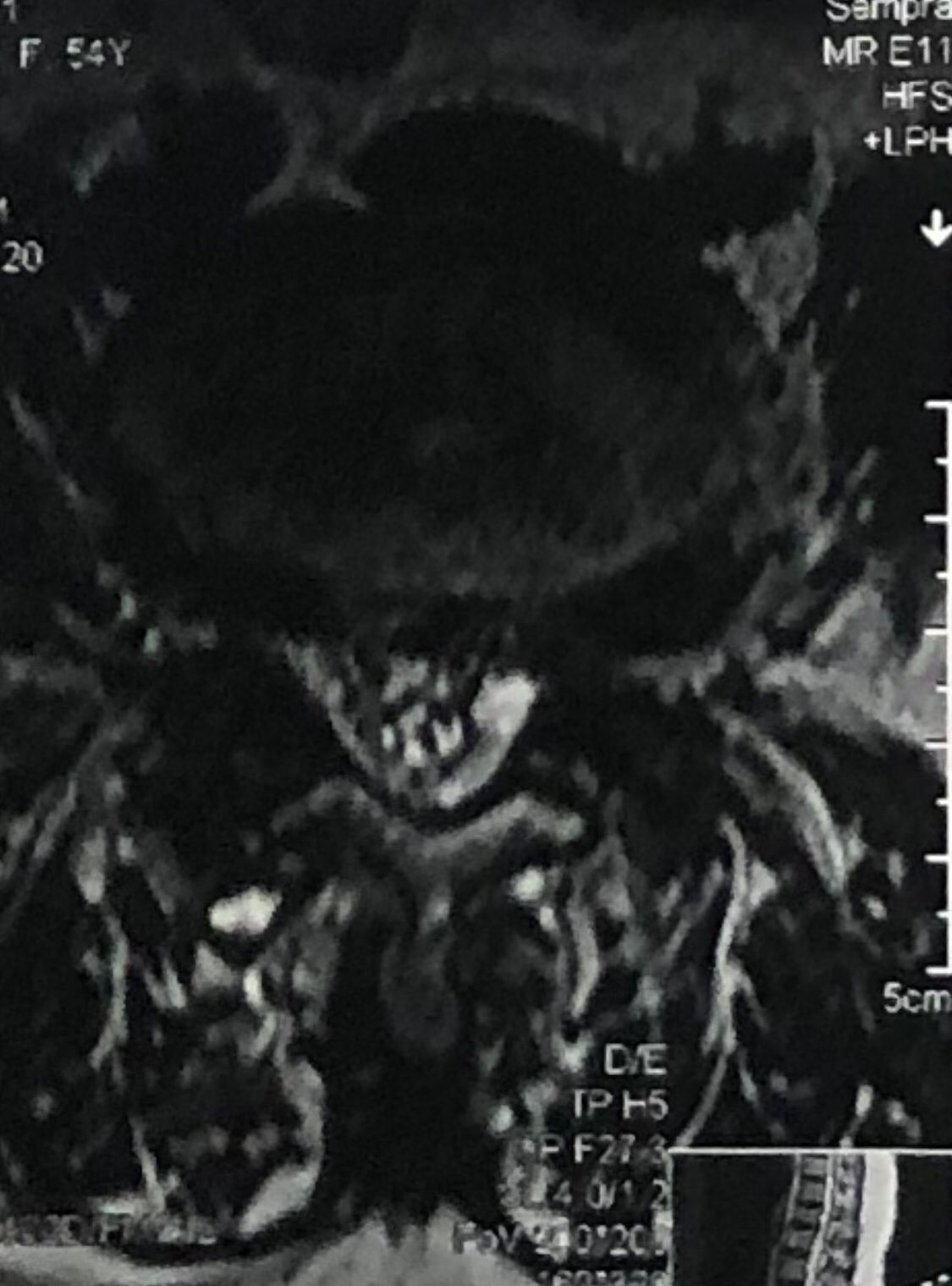
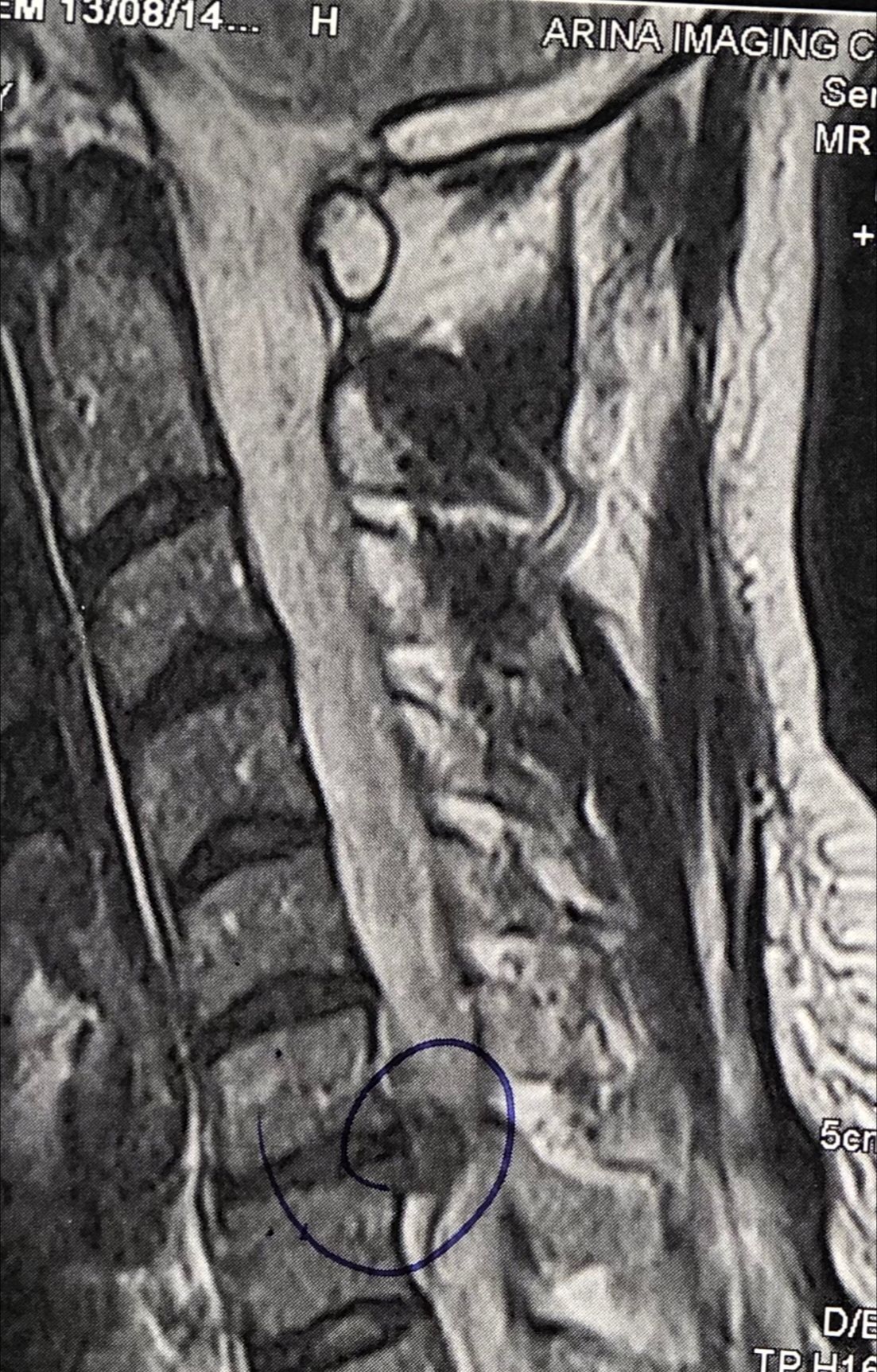
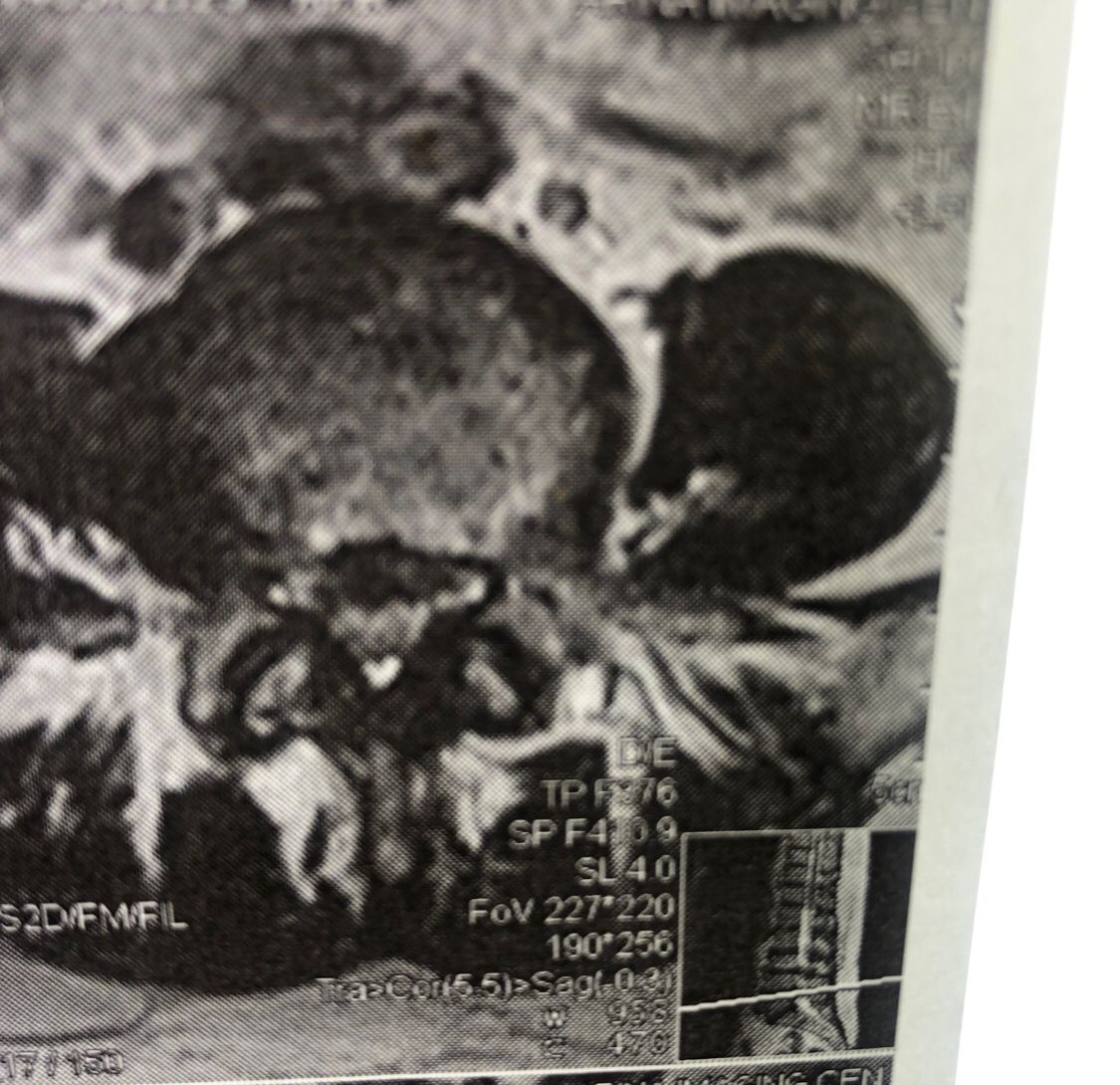
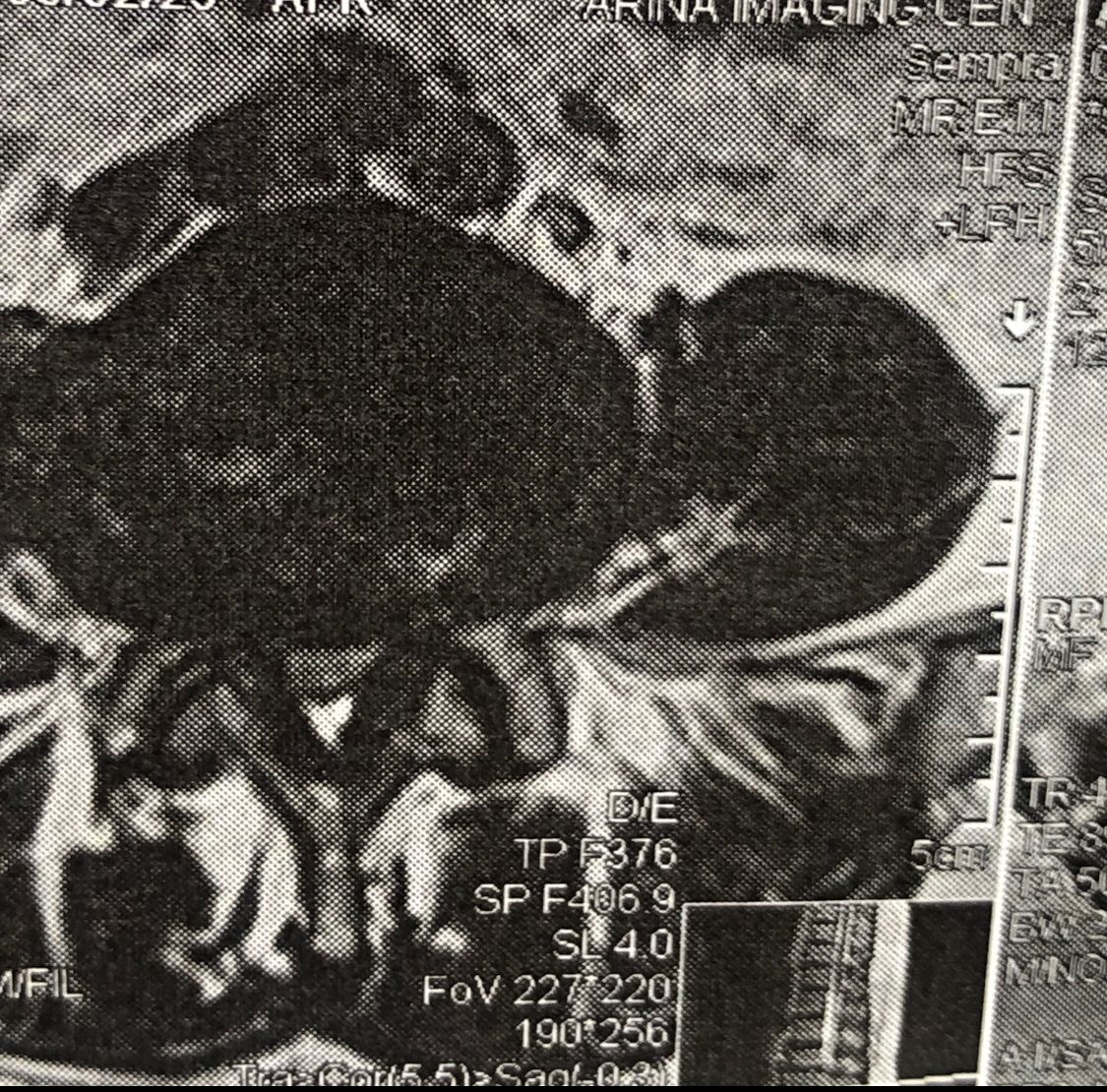
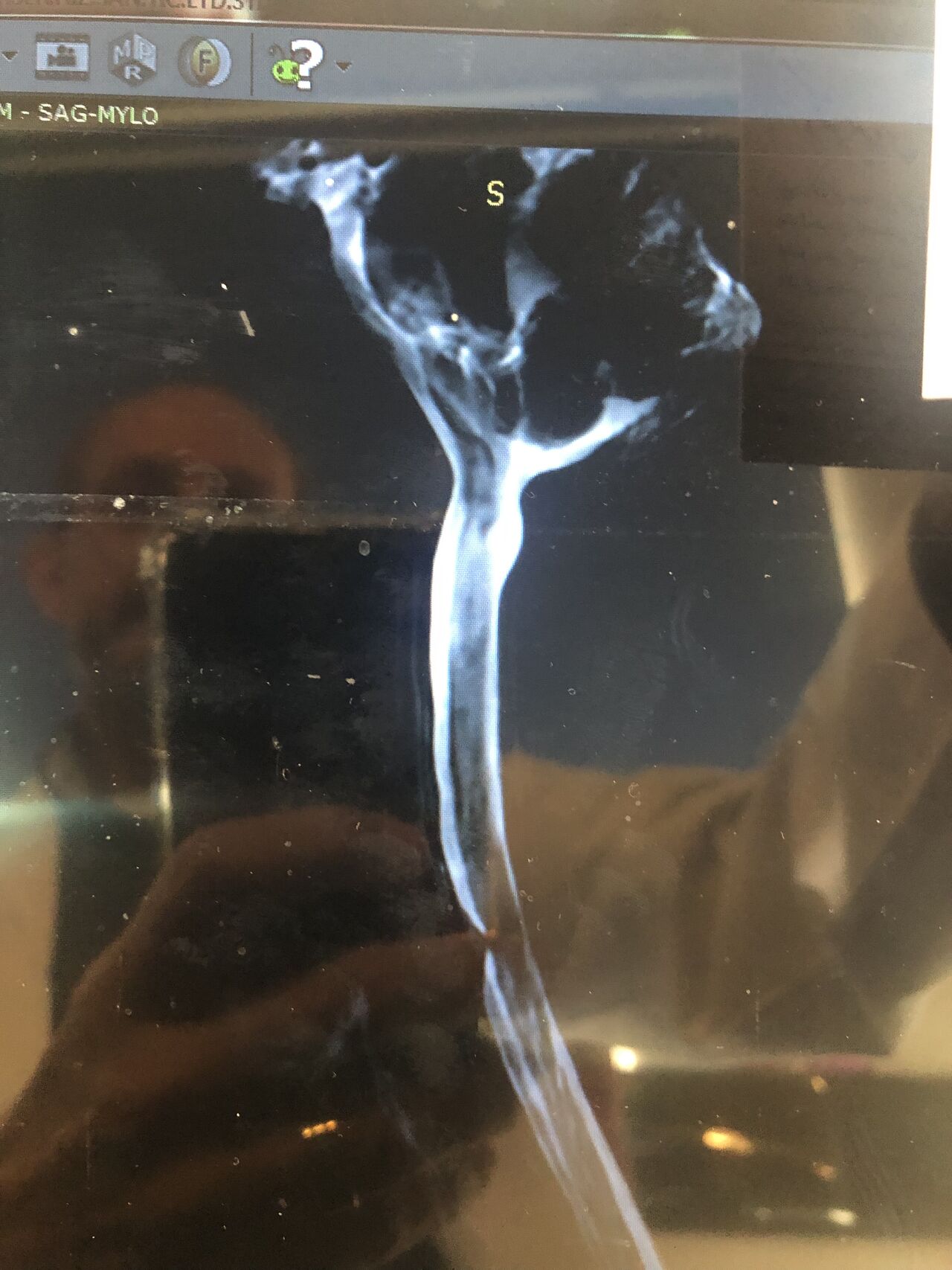
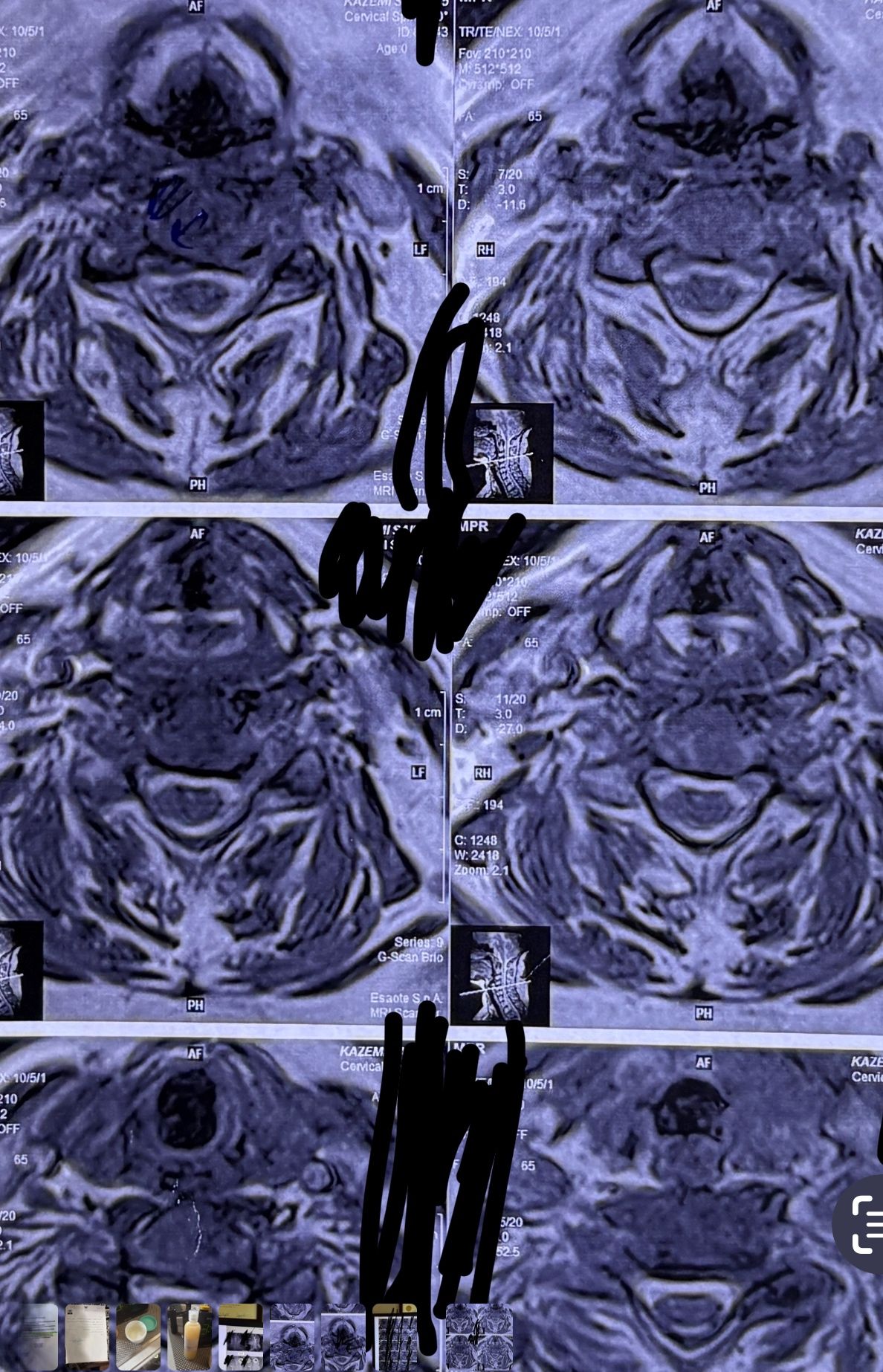
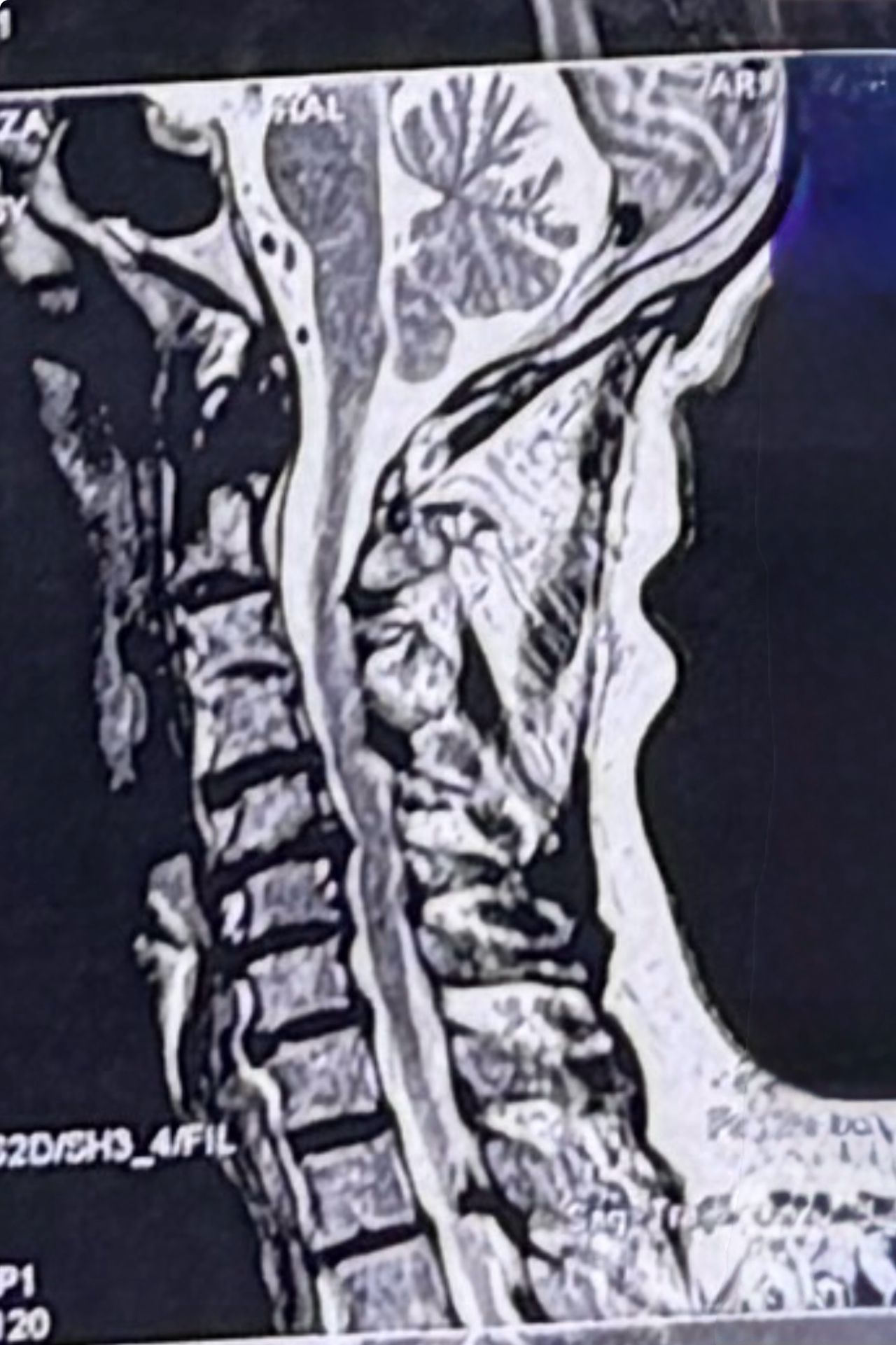
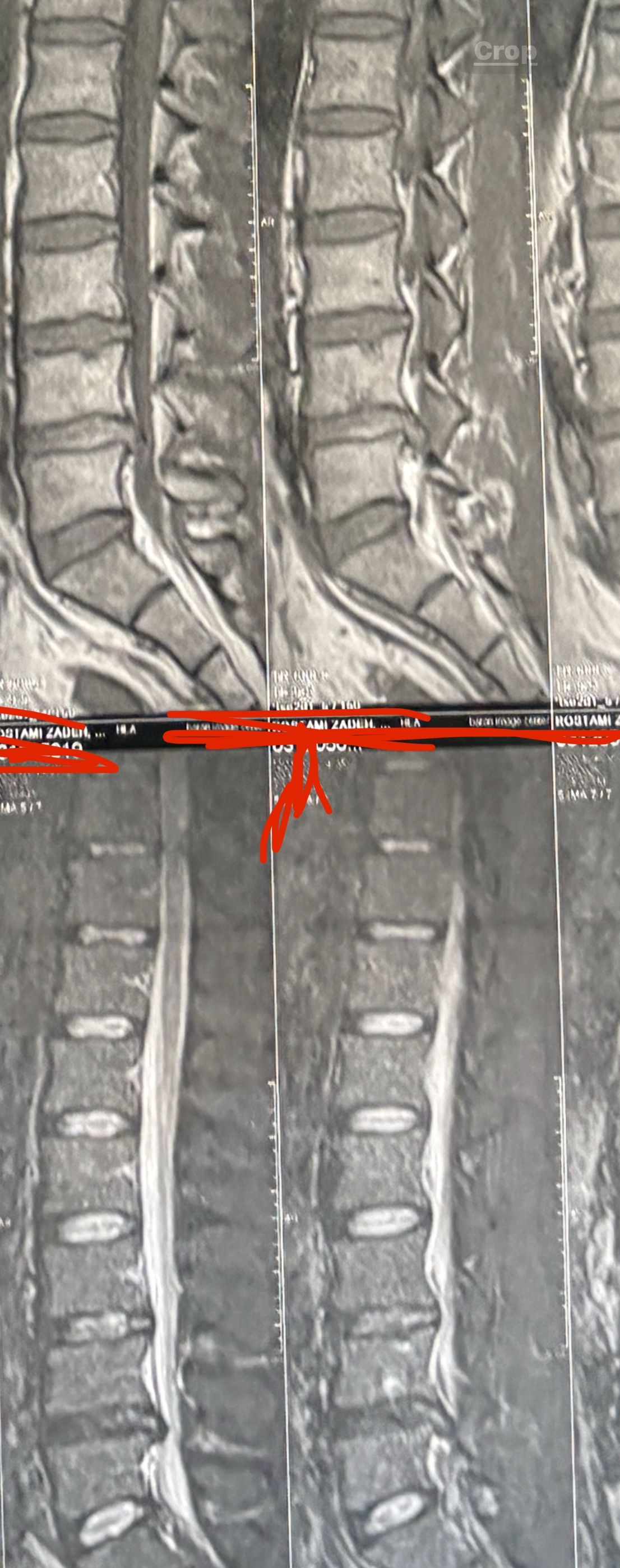
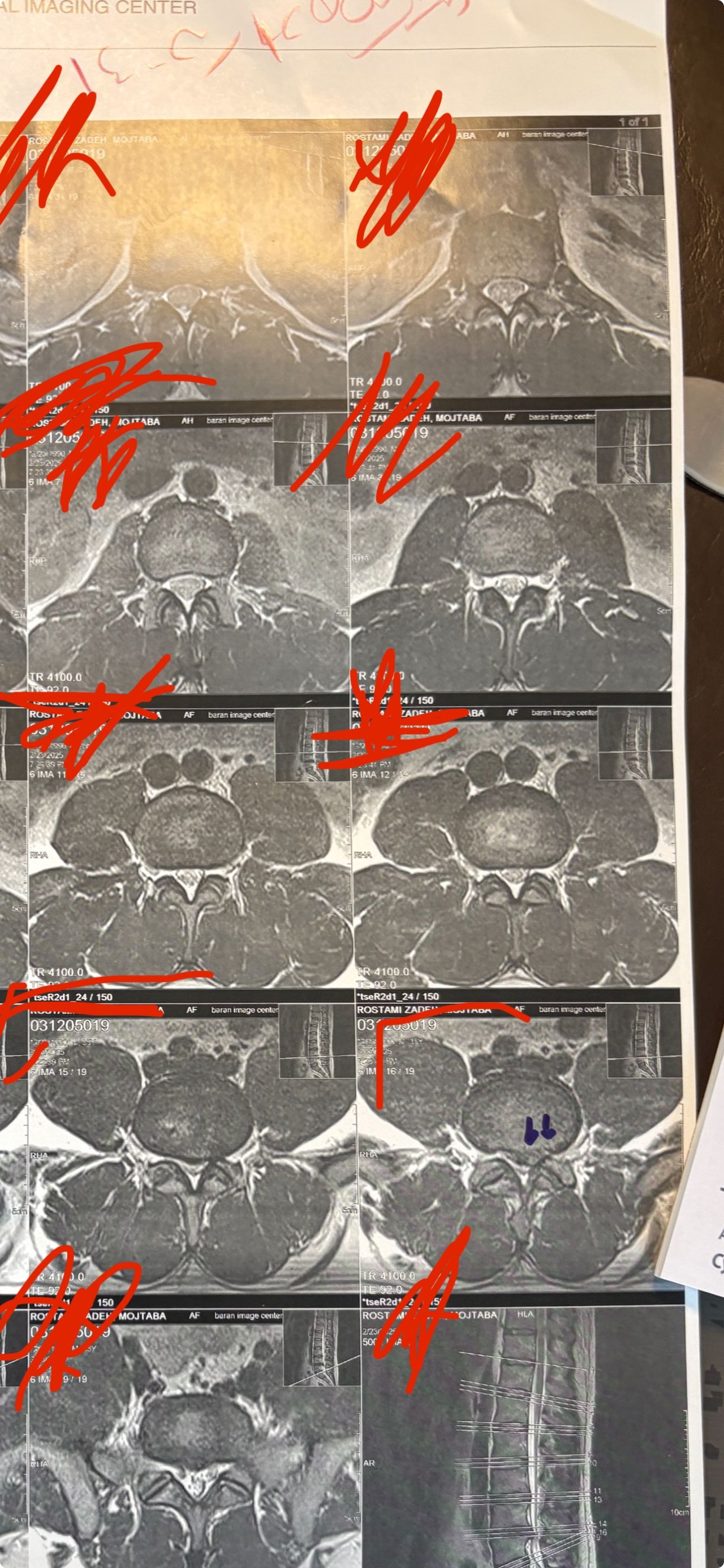
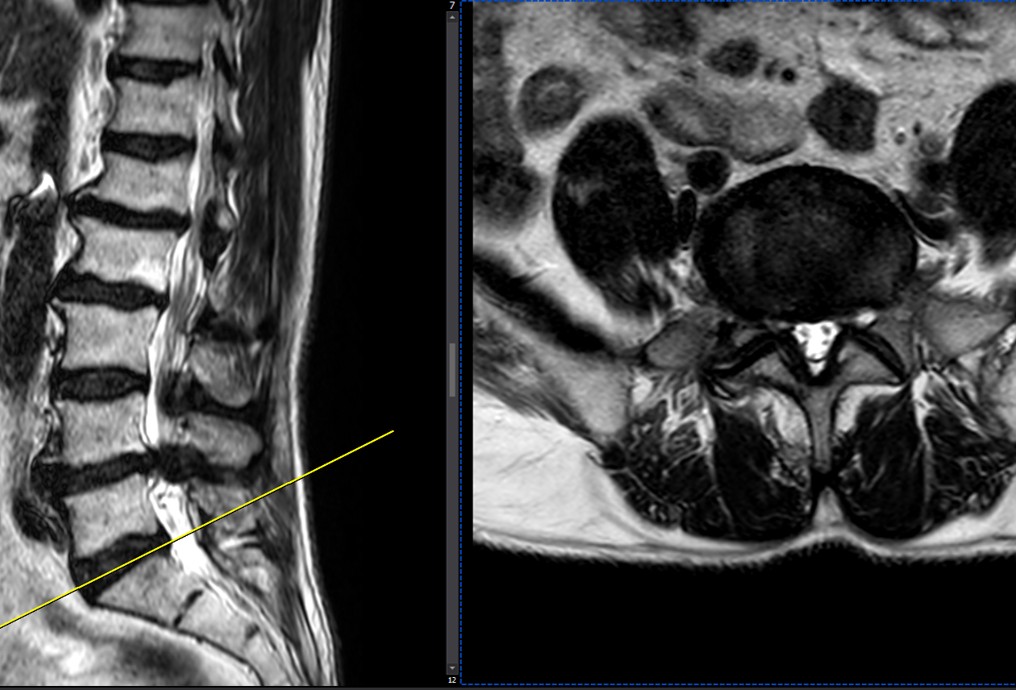
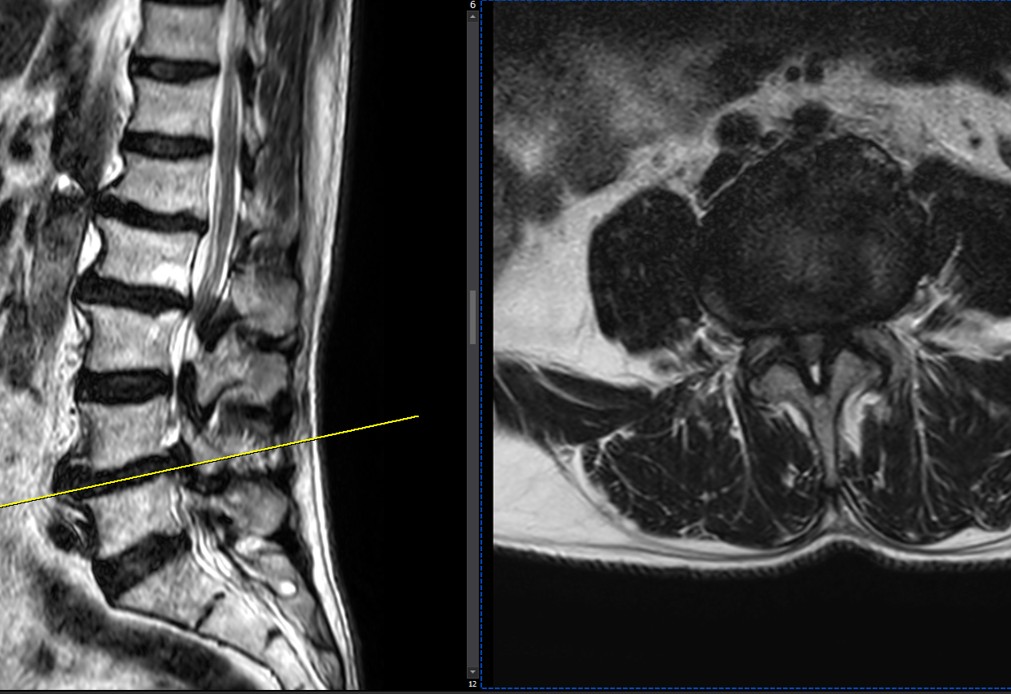
41 years old man presented to my clinic in October 2023 with acute and sever R neck pain with radicular pain to his R upper extremity along C6 dematom since 2 weeks ago. Examination didn’t show any upper motor signs. Was suggested urgent surgery
I ordered EMG/ NCV : showed mild R C6, C7 irritation without any active axonal loss
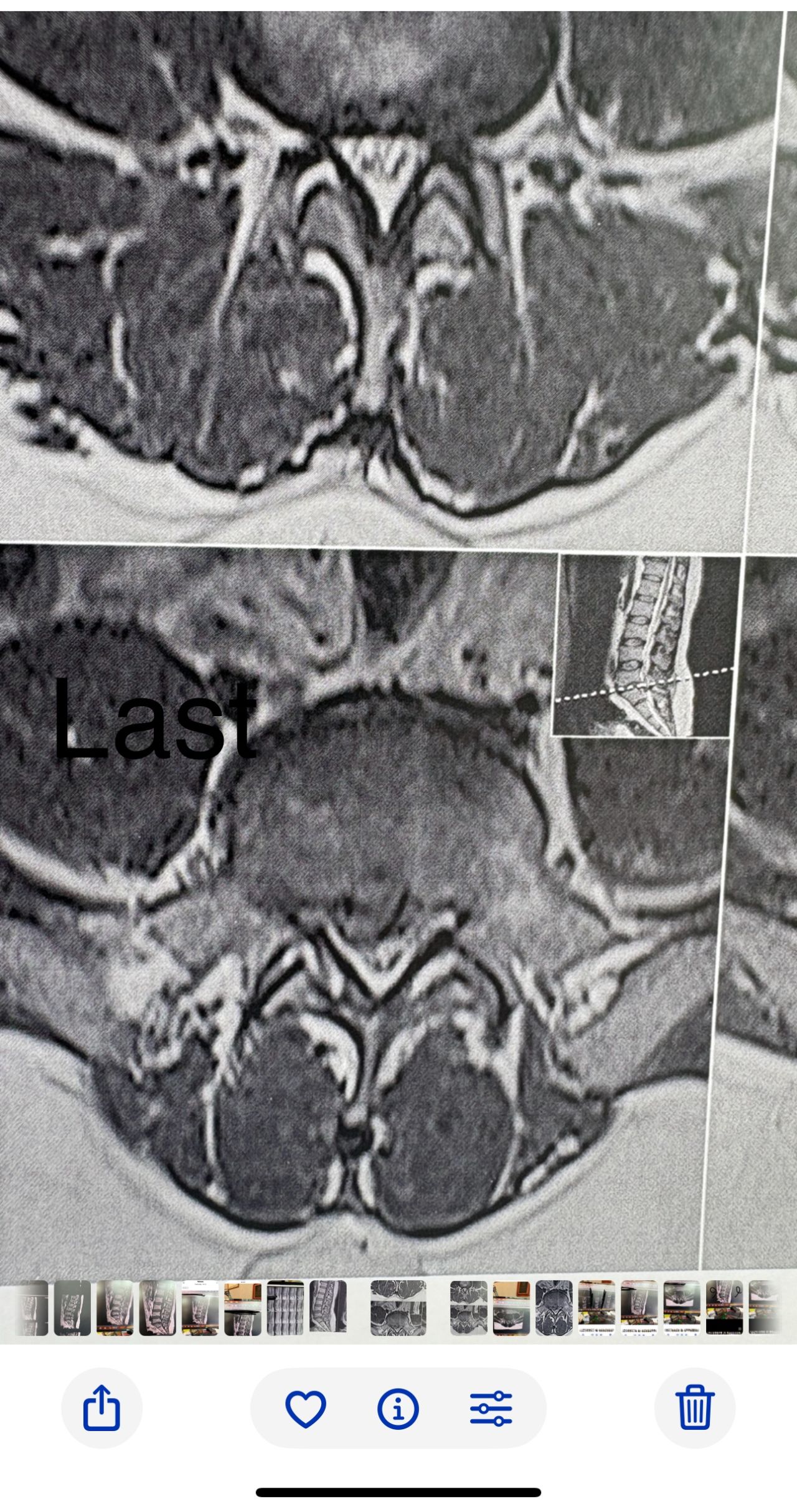
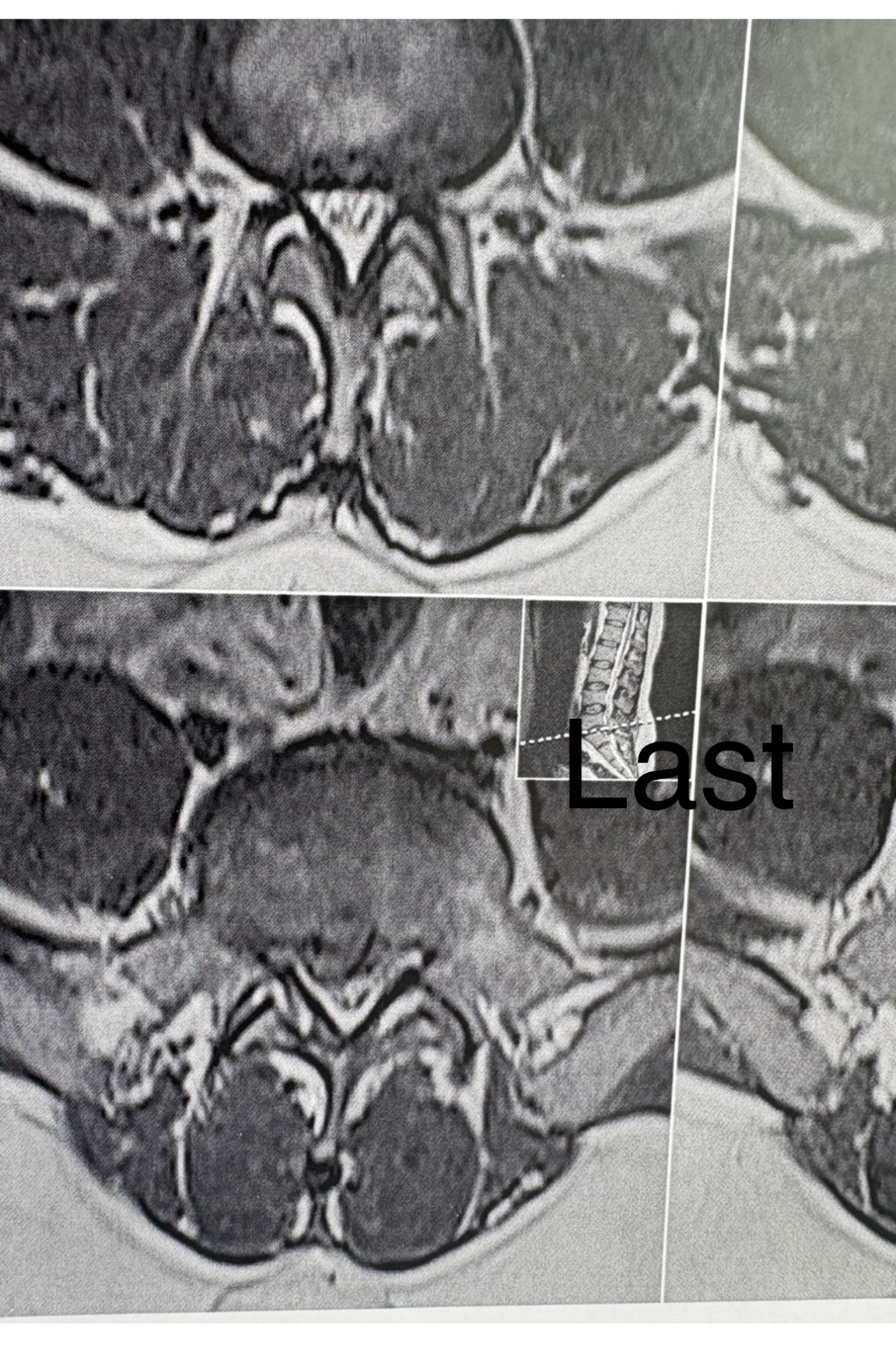
In his MRI was reported R. para R. IVF Massive extrusion. I decided to control his pain and manage this patient with reevaluation of patient every other session. For 5 sessions i just used acupuncture and laser and IFC and mild adjustments to his R. T3-T7 and mild arthosteem to above and below involved segment. Cervical adjustment considered contraindicated for this patient. From session 6th- 8th i started to use mild/gentle cervical decompression. He used soft cervical collar all the time. His pain decreased by 80 percent
I gave him cervical traction pump to be used 3-5 times per day at home for the next 3 months and i released the patient. He was evaluated every week once for one month and after that every 2 weeks. After 3 month I repeated MRI. Size of the herniated disc was reduced greater than 50 percent. Asked him to do another mri in 6 months
In general: Precise selection of the patients, examination,diagnosis, plan of management, reevaluation and treatment can be done by doctors of chiropractic for the patients with spinal disc herniation and stenosis Moreover giving reasonable time to these kind of patients under direct supervision by their chiropractic doctors can prevent unnecessary surgery. Proper selection of these kind of patients is another important fact that can be done precisely by chiropractors.
MRIs before and after proper management of this patient:
Case 17
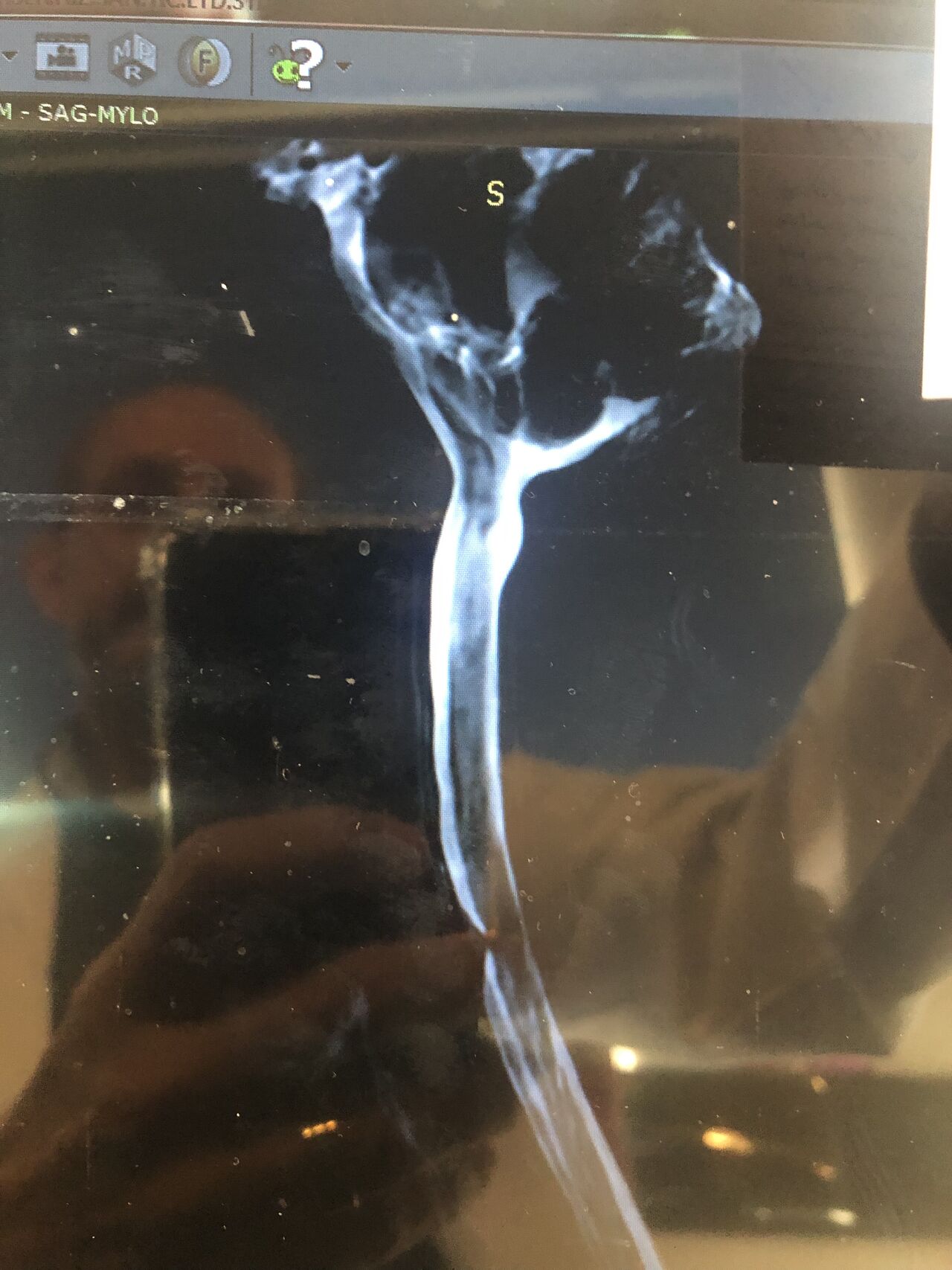
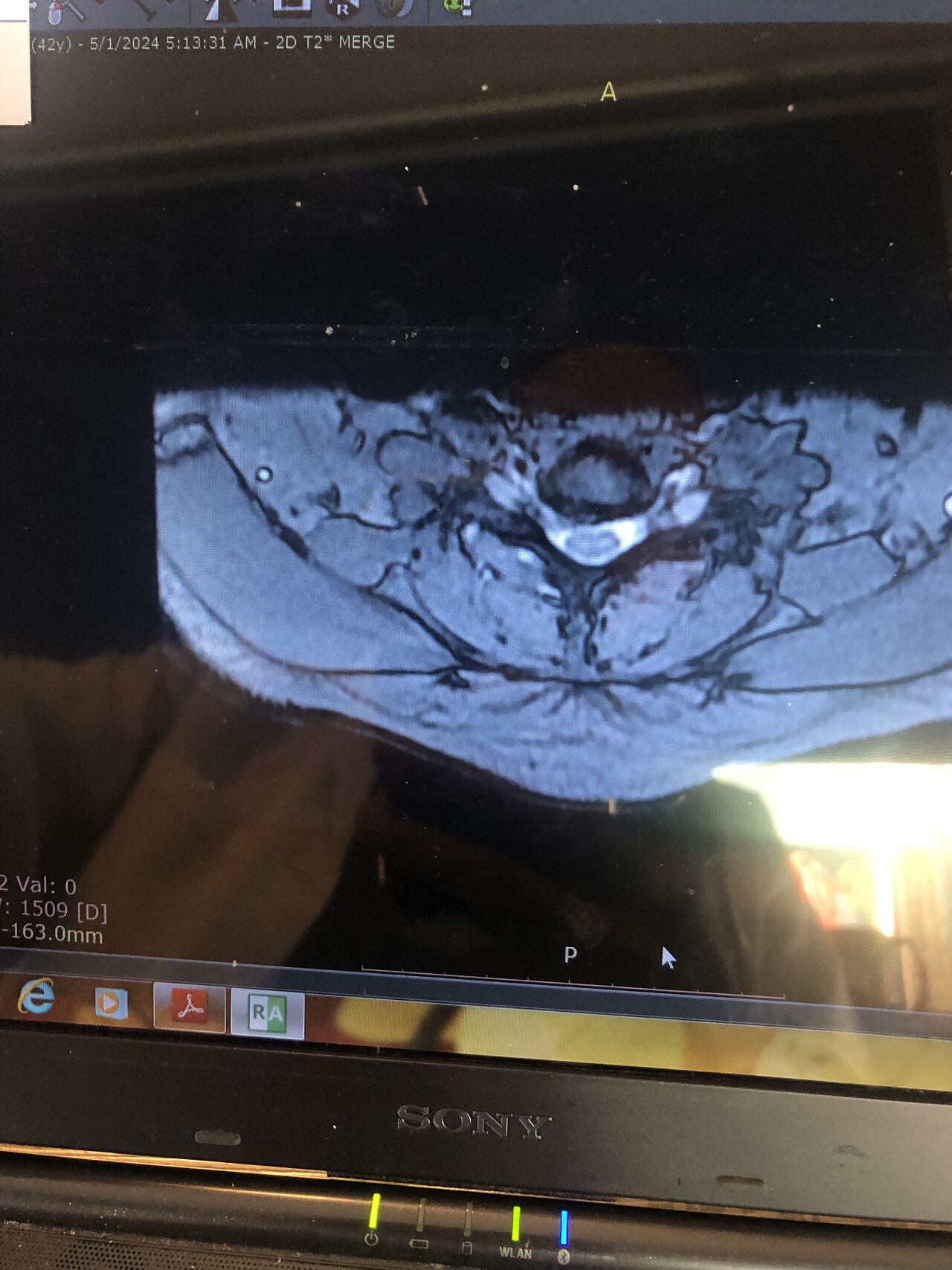
40 yrs old female patient presented to my clinic 2 hrs ago on May 18/2024 with severe neck and R upper extremity pain along C6 dematome. Had 12 sessions of PT with almost 20 percent improvement in her pain. Still has severe pain. I ordered EMG/ NCV( result showed moderate R c6 radiculopathy with no axonal loss)
Her mri is posted. i have started her treatment with acupuncture and very gentle cervical decompression. In 3 months her mri will be repeated
Case 18
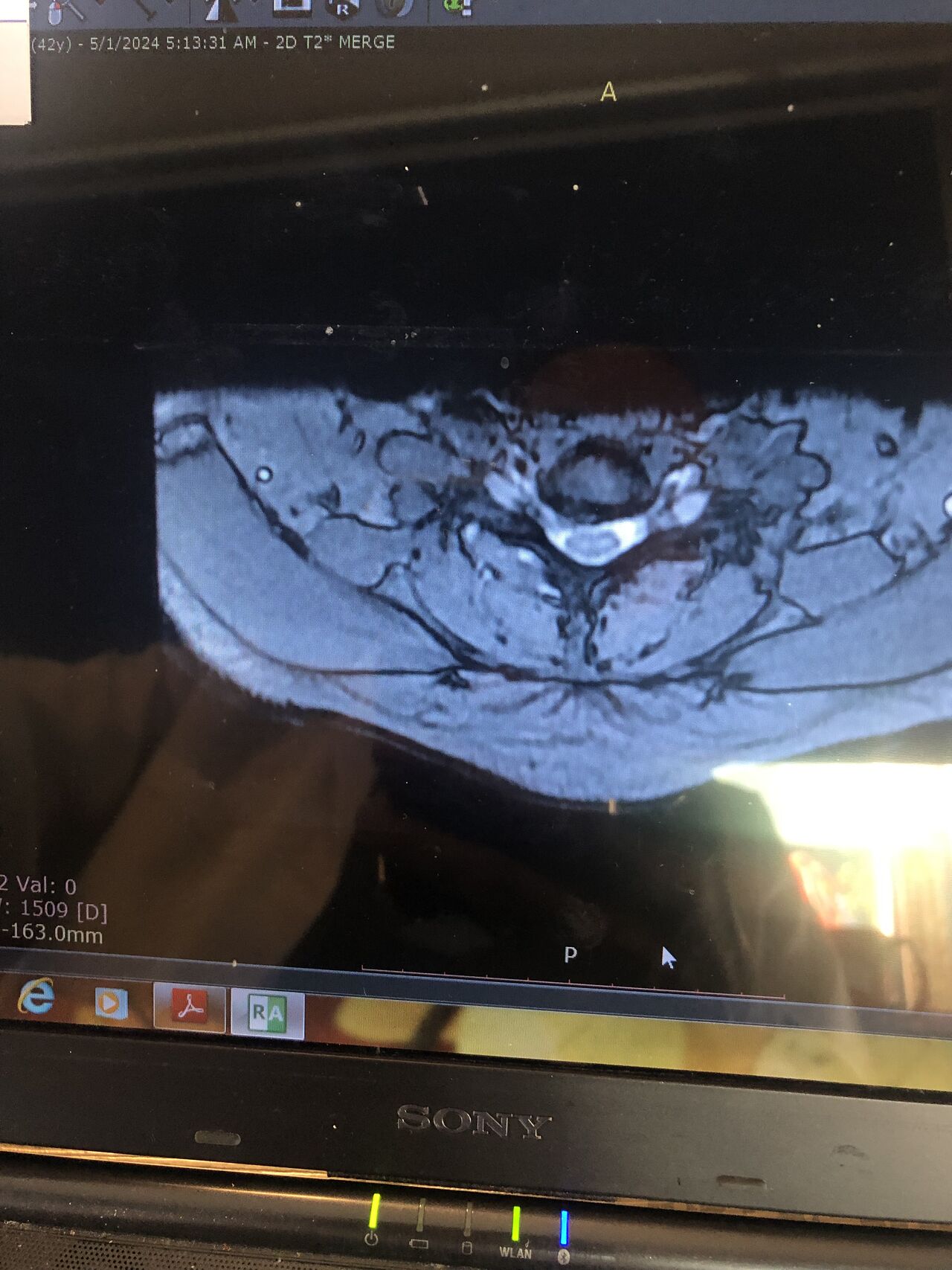
59 yrs old female just presented to my office2 hrs ago with severe R gluteal pain. No leg radiculopathy. Walking is pain free . Just aggravates by sitting. Doctors of chiropractic are able to manage these patients
What would be your plan for management? Do you adjust this patient?
Case 19
59 yrs old female today was presented to my office few days ago with low back pain in walking. Had history of fall 4 years ago which was resulted in L 3 fracture. She had sement injection in L3.
I ordered DEXA ( had osteopenia in hip) and dynamic lumbar spine x ray Please mention what would be your plan of management. If you decide to give her treatment what kind of treatment(adjustment or decompression or other treatments)whould be suitable for her? Doctors of chiropractic can decide and come up with good plan of management and treatment for these patients and are well trained when they have to refer these patients for surgery or pain management clinics. Proper selection of these kind of patients is another important fact that can be done precisely by chiropractors.
Case 20
59 yrs old female just presented to my office2 hrs ago with severe R gluteal pain. No leg radiculopathy. Walking is pain free . Just aggravates by sitting. Doctors of chiropractic are able to manage these patients
What would be your plan for management? Do you adjust this patient?
Case 21
40 yrs old female patient presented to my clinic 2 hrs ago on May 18/2024 with severe neck and R upper extremity pain along C6 dematome. Had 12 sessions of PT with almost 20 percent improvement in her pain. Still has severe pain. I ordered EMG/ NCV( result showed moderate R c6 radiculopathy with no axonal loss)
Her mri is posted. i have started her treatment with acupuncture and very gentle cervical decompression. In 3 months her mri will be repeated
Case 22
55 yrs old female was my patient since 15 years ago i saw her 11 years ago again due to neck pain she had C5-7 small protrusions with C3-4 bulge
Presented to my office few days ago on june 082/2025 with severe neck pain and pain radiation to the R upper extremity
She was going to yuga class for several years yand has done the following exercise a lot:
Yoga candel move which is so harmful for neck
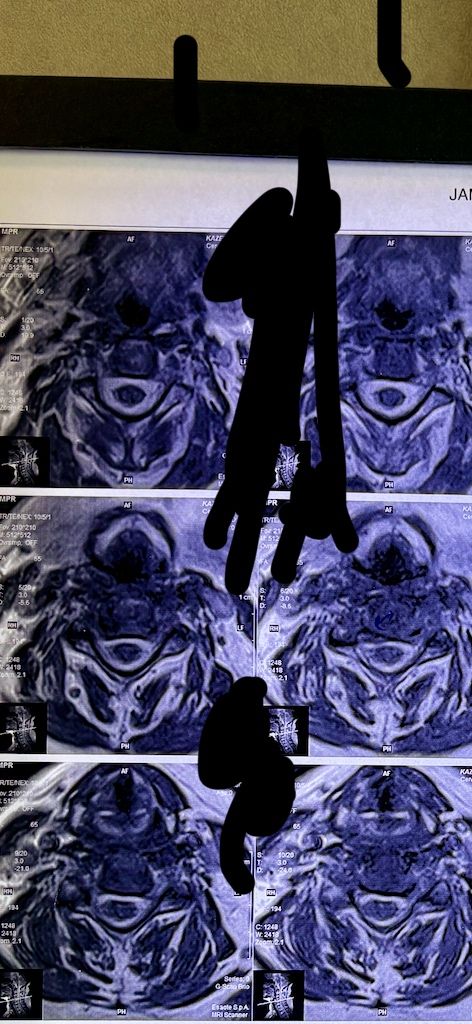
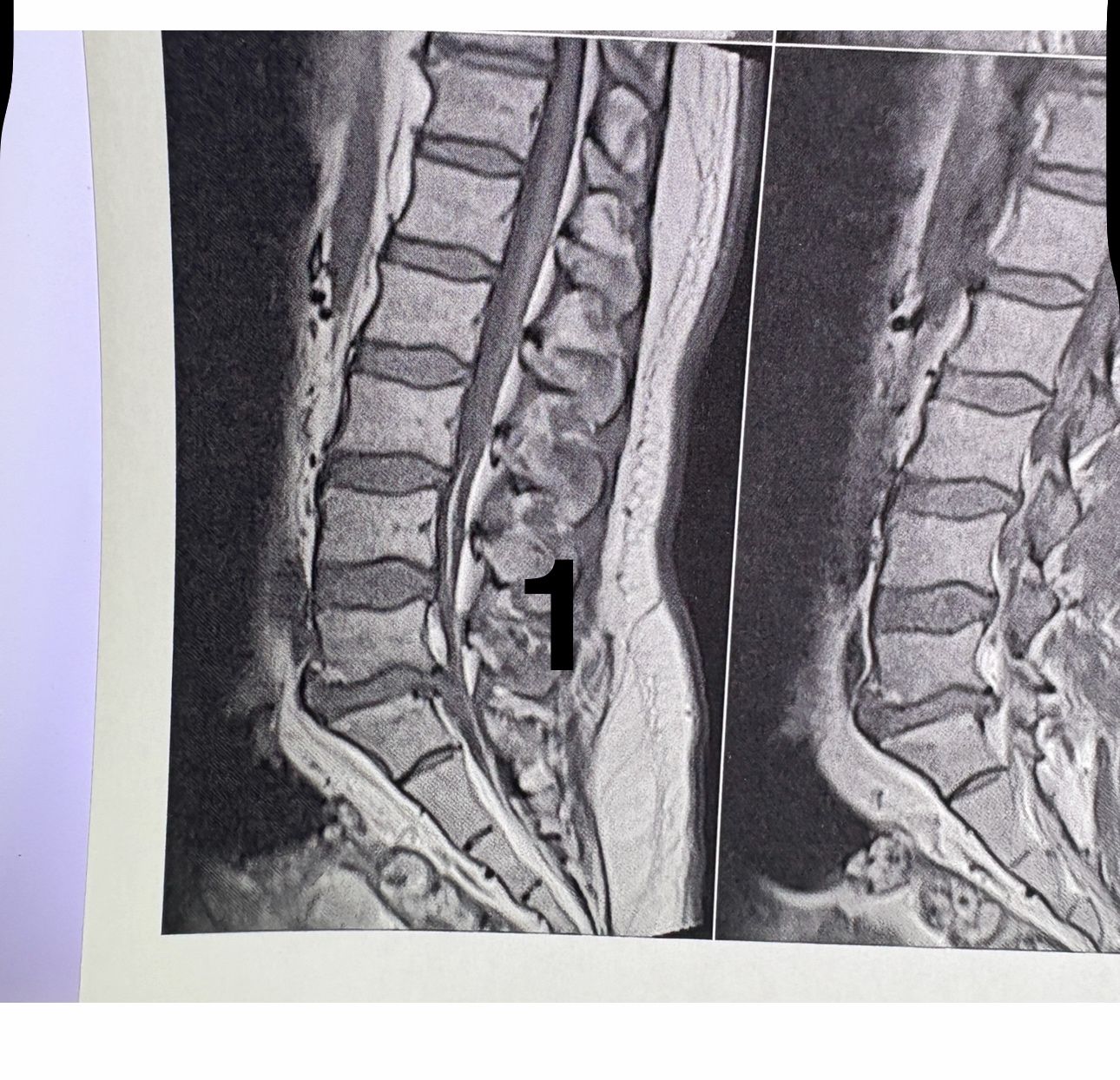
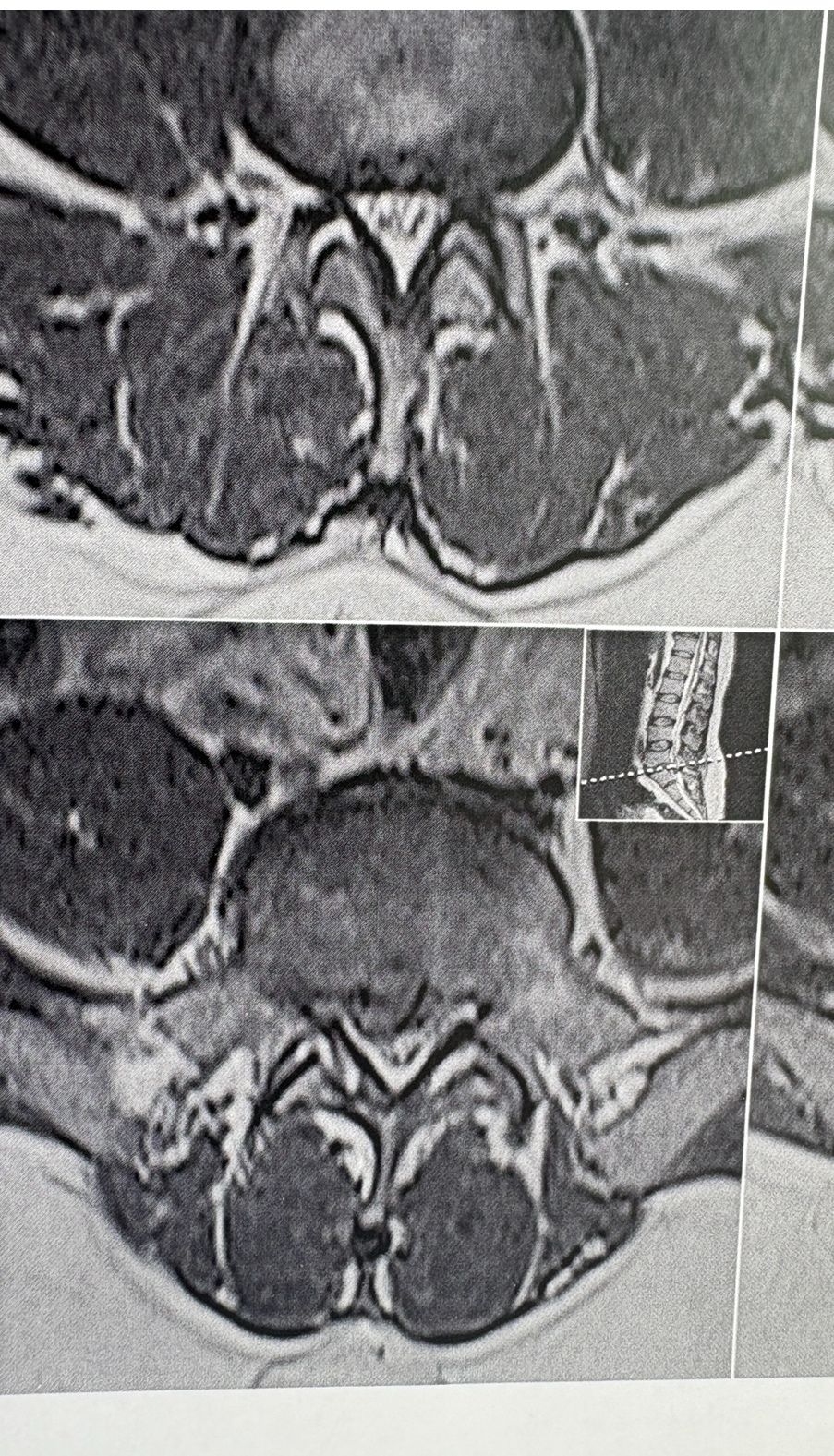
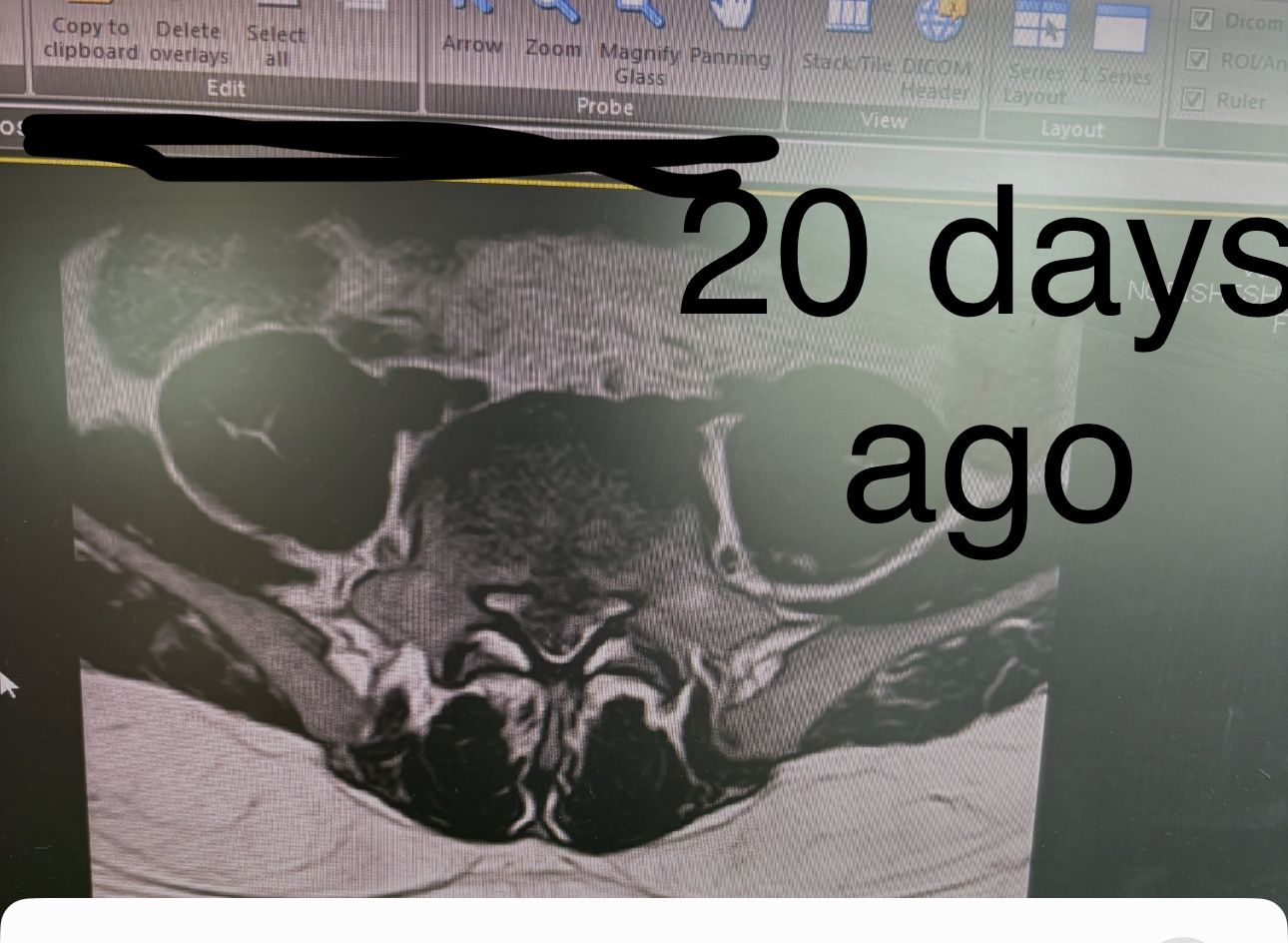
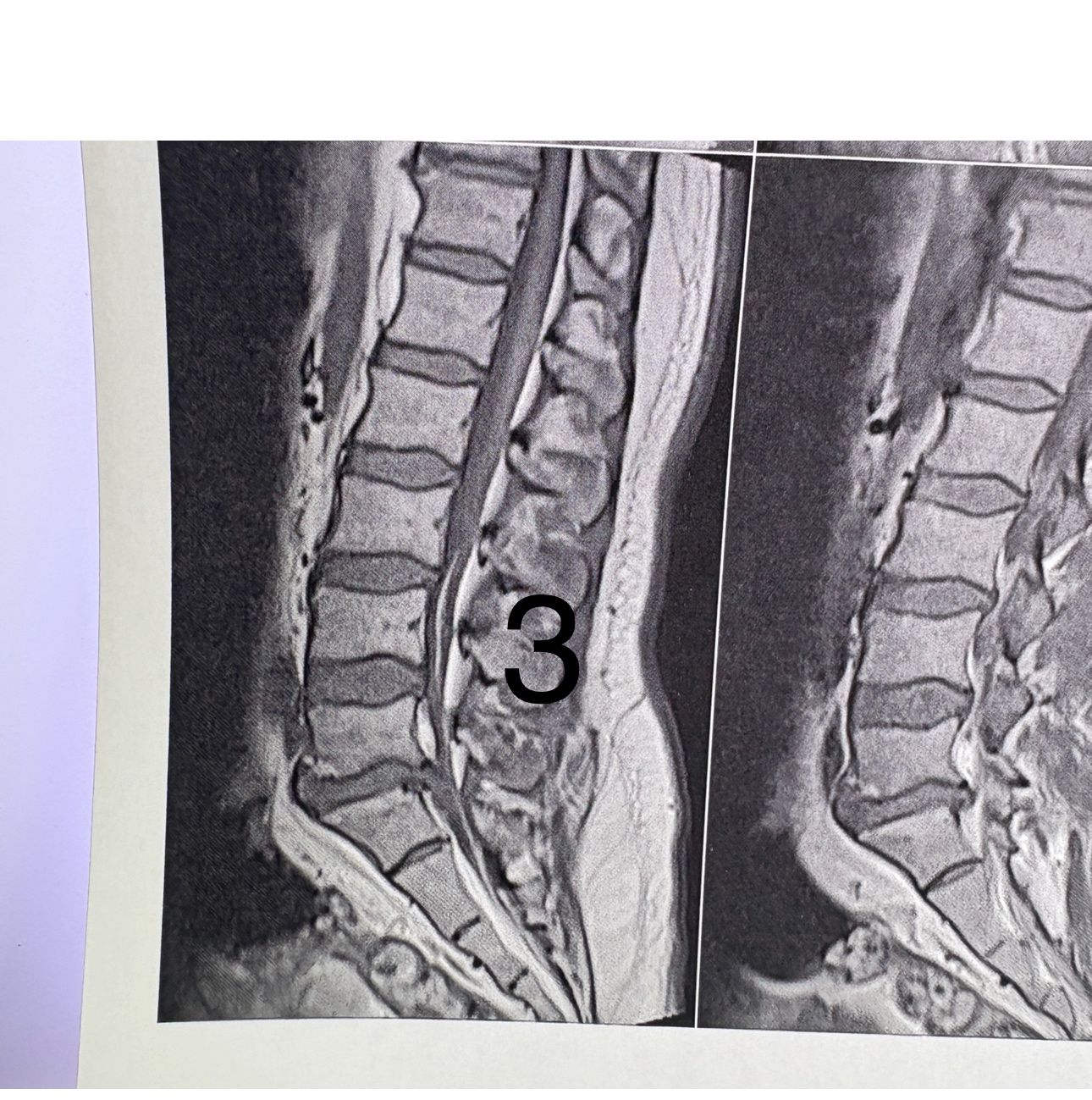
Case 23
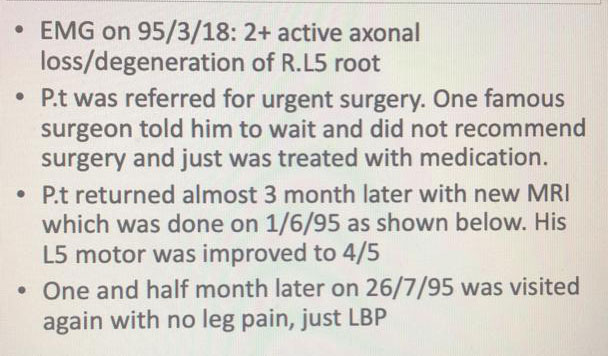
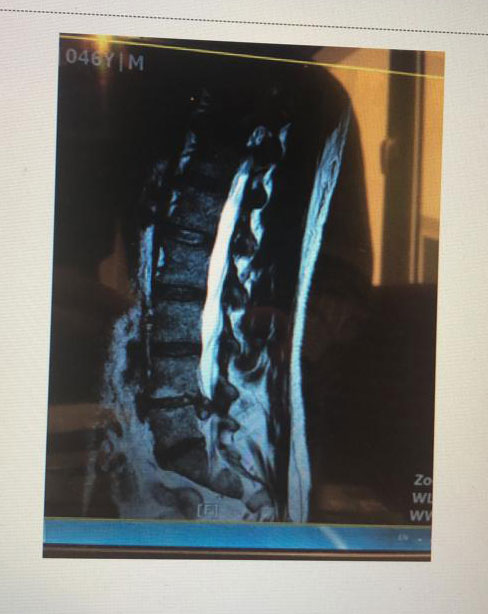
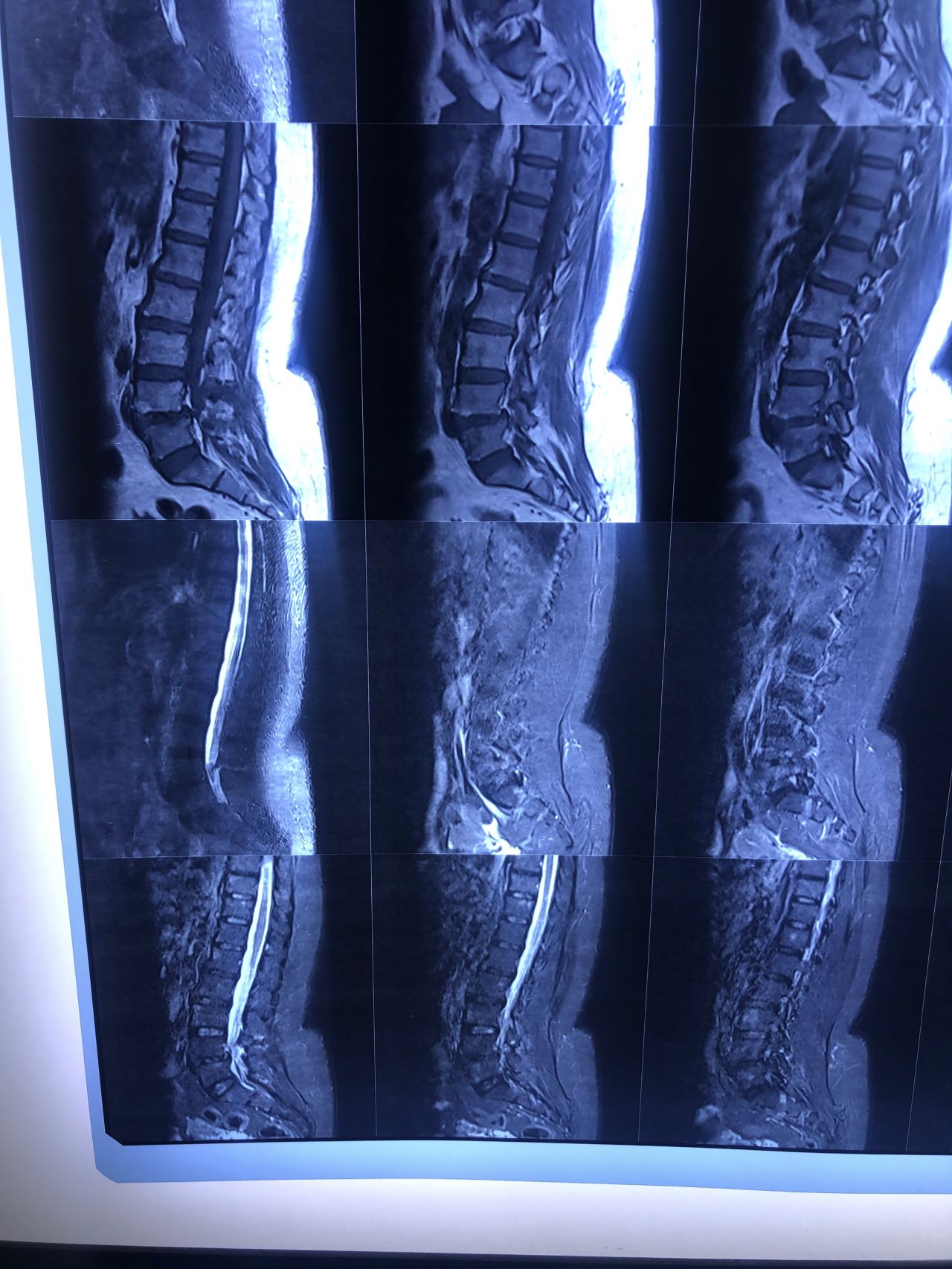
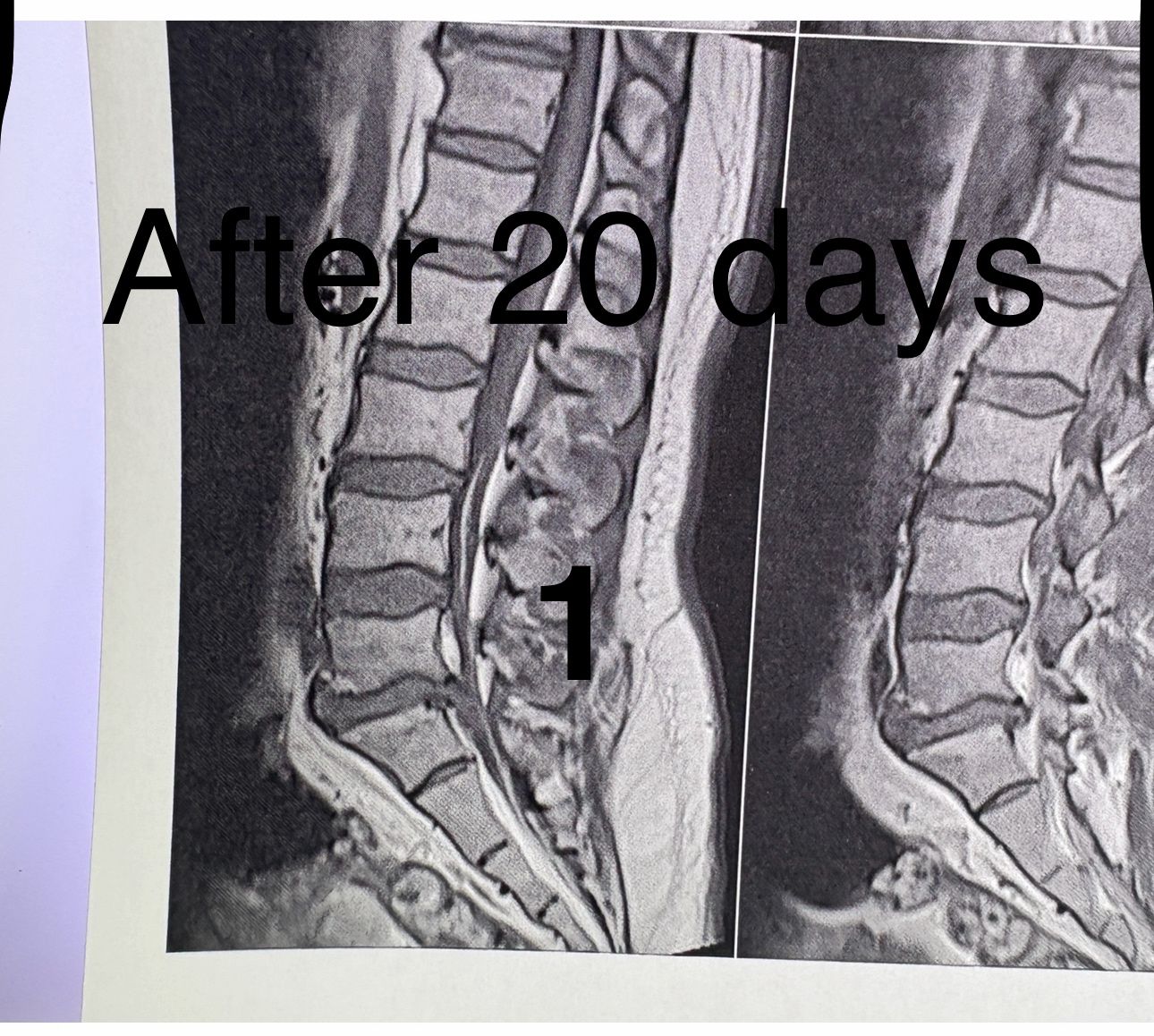
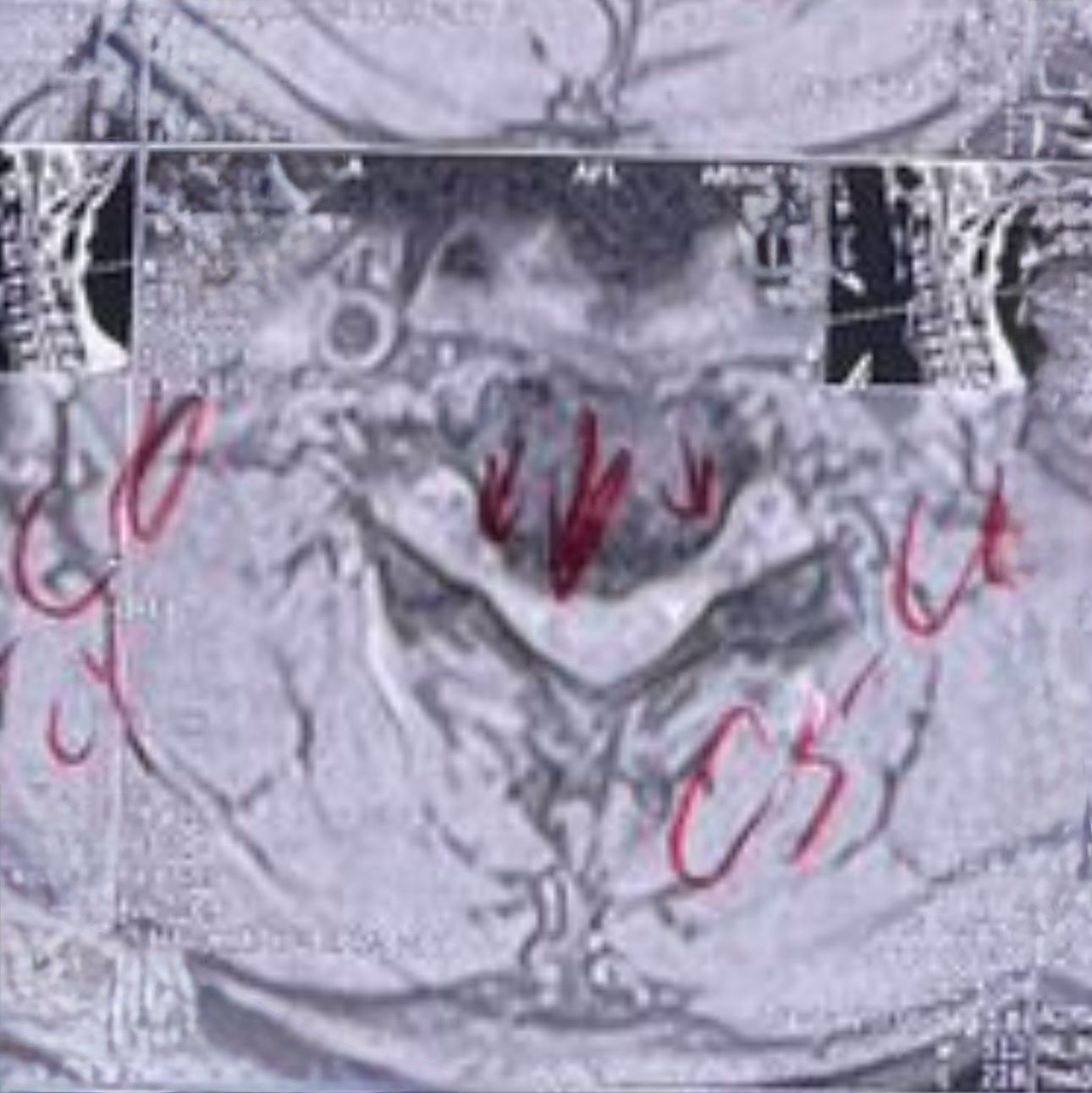
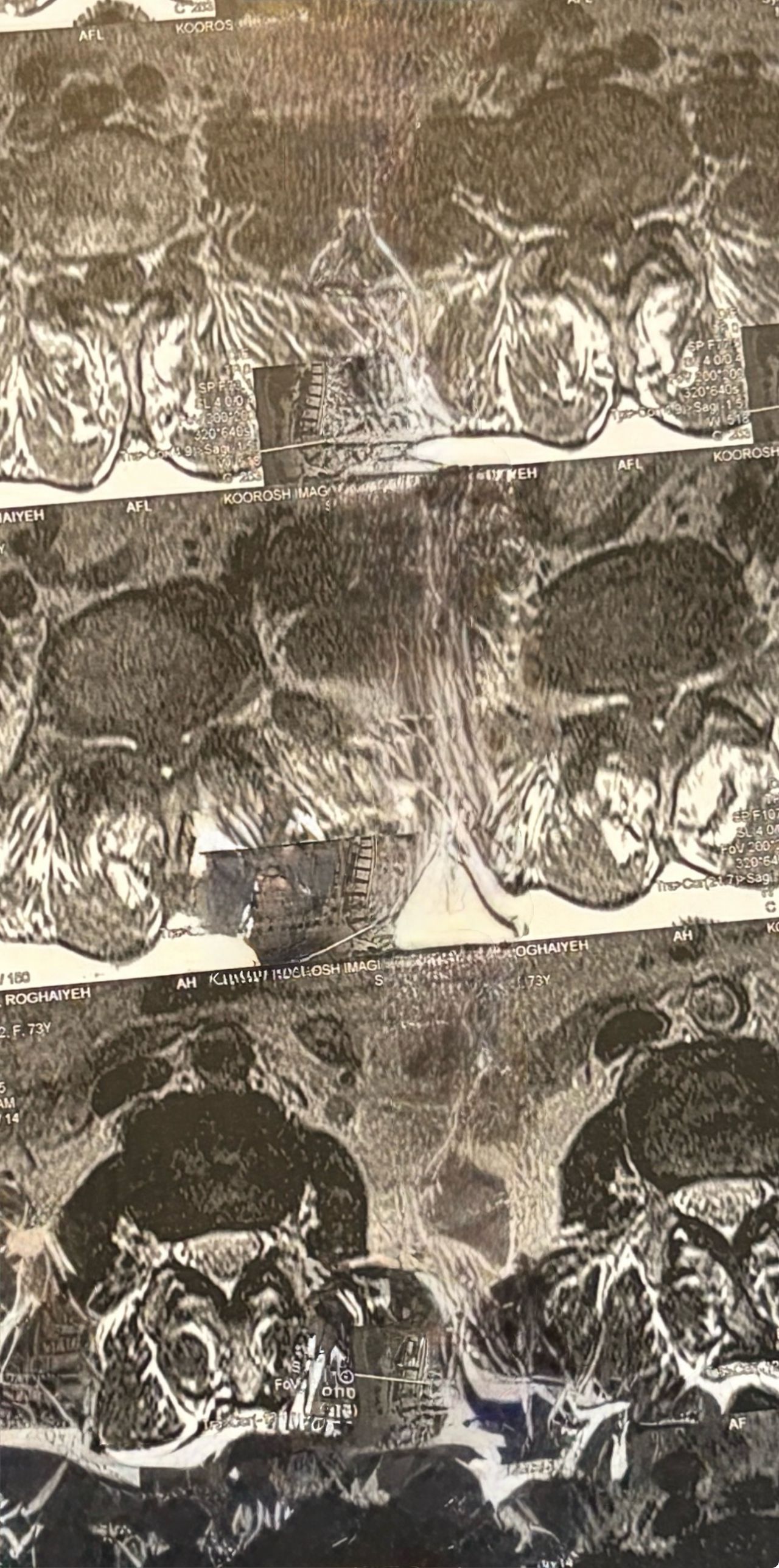
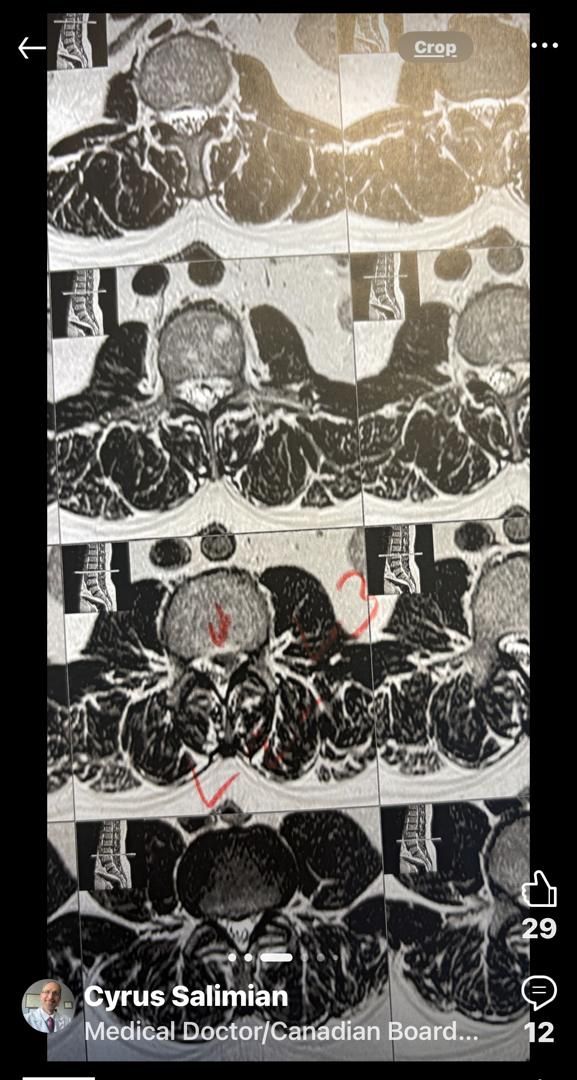
40 yrs old male patient presented to my office who had severe R gluteal pain and radicular pain along R L5-S1 now pain has reduced by 80% in his motor exam had R big toe L5 motor reduced to 4+\5 and R S1 DTR was 0 while L S1DTR was 1+
We did EMG/NCV which showed Mod- sever R L5 S1 irritation without any active axonal loss
I had to decide to refer him for surgery or not patient didn’t have any treatment meanwhile
I ordered new L/S mri
I posted his new mri and old mr
Which was 20 days ago and have posted all below
The first 12 mris had been done 20 days ago
After those first 12 MRIs i have posted new MRIs which were done yesterday
After seeing his new mri and emg/ncv and getting sure his neurological deficit is not active and progressing i told patient he doesn’t need surgery at this time and released him with some advices and exercises
Keep in mind when patient is 80-90 percent pain free and stable i would never give treatment to them just give exercises and follow up their condition
Case 24
86 years old male patient was referred to me by a neurologist one week ago for evaluation and choosing proper plane of management ( he trusts me in handling patients properly)
Patient has had severe LBP for the last 2 weeks
Had history of prostate cancer surgery 20 years ago
What are your DDxs and POM?
Case 25
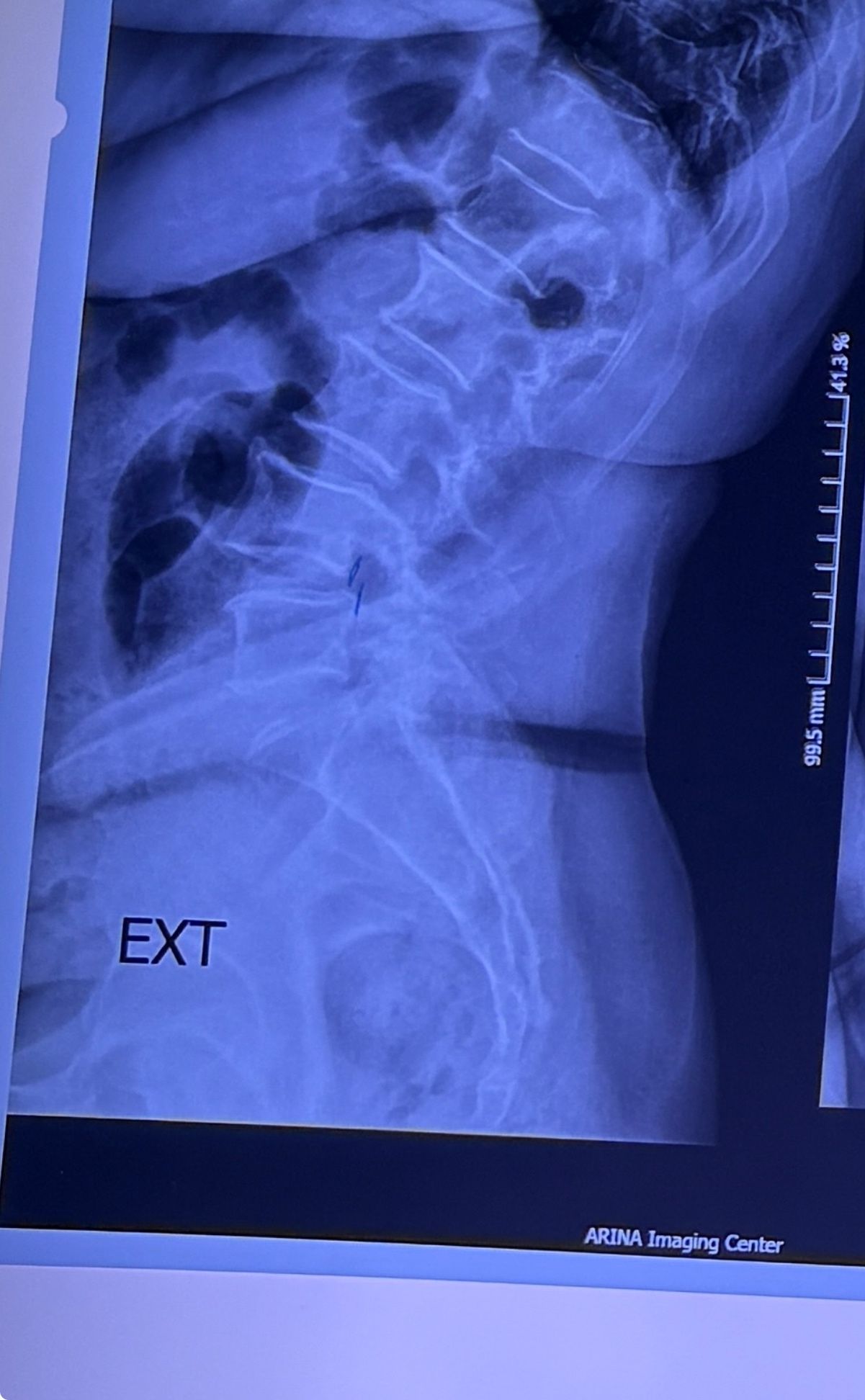
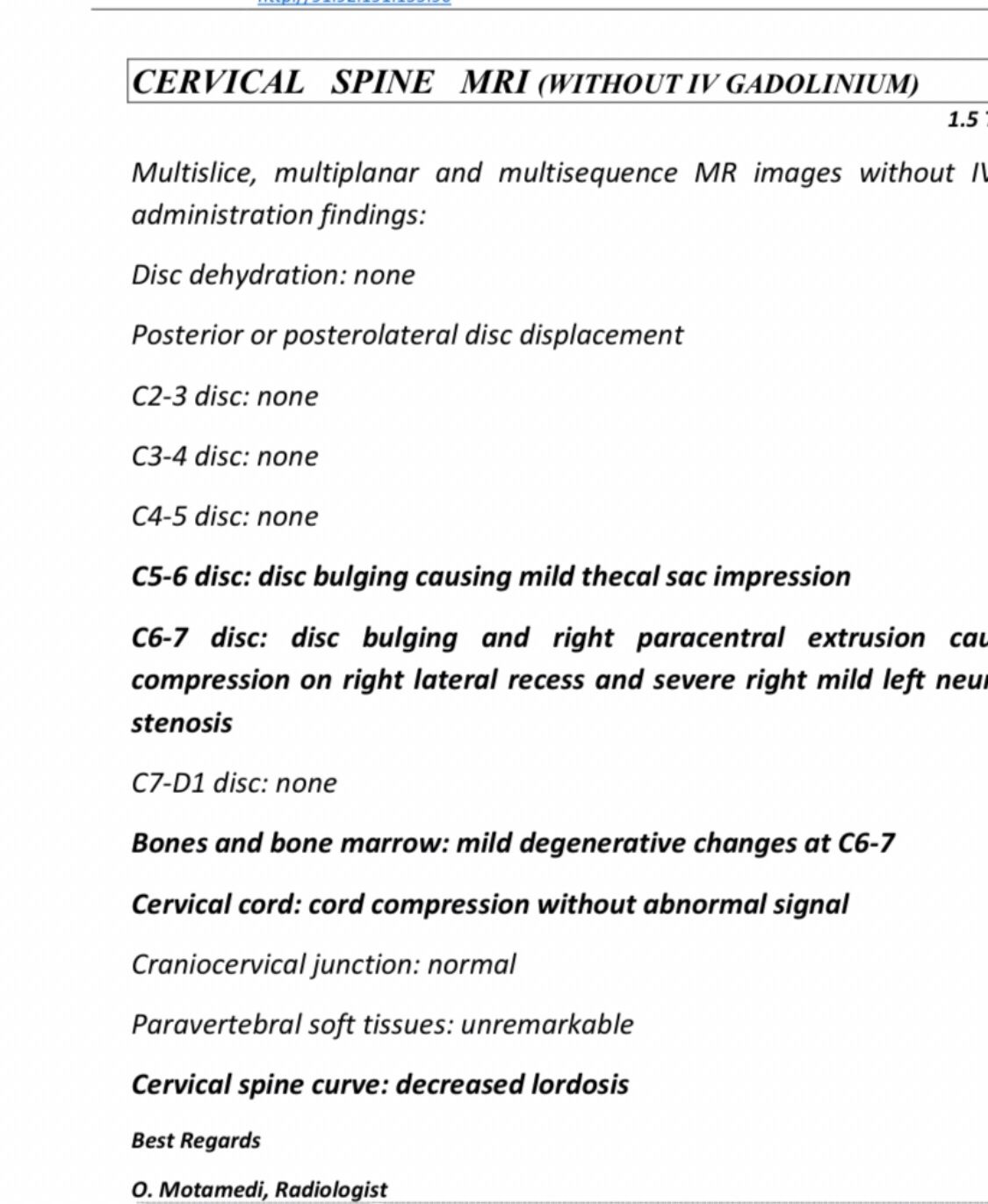
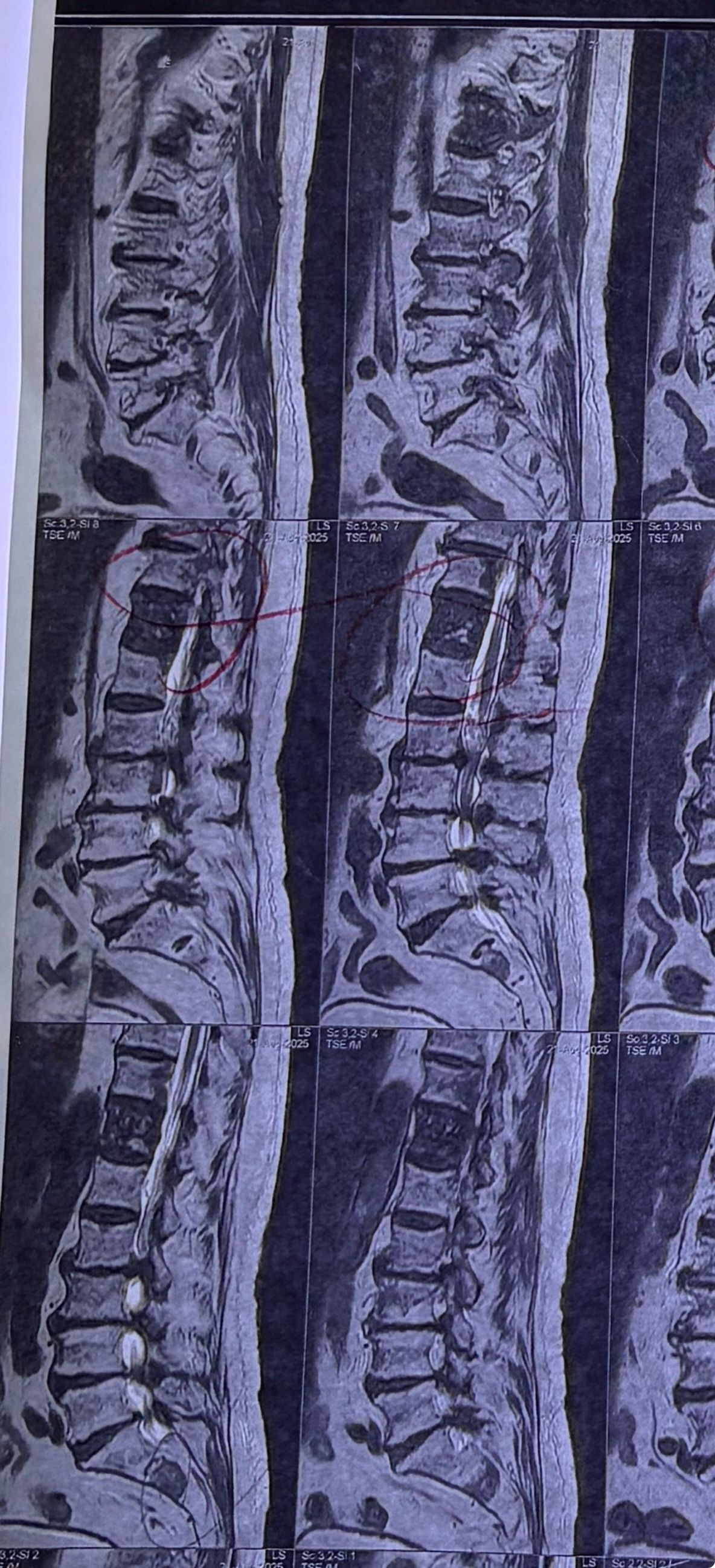
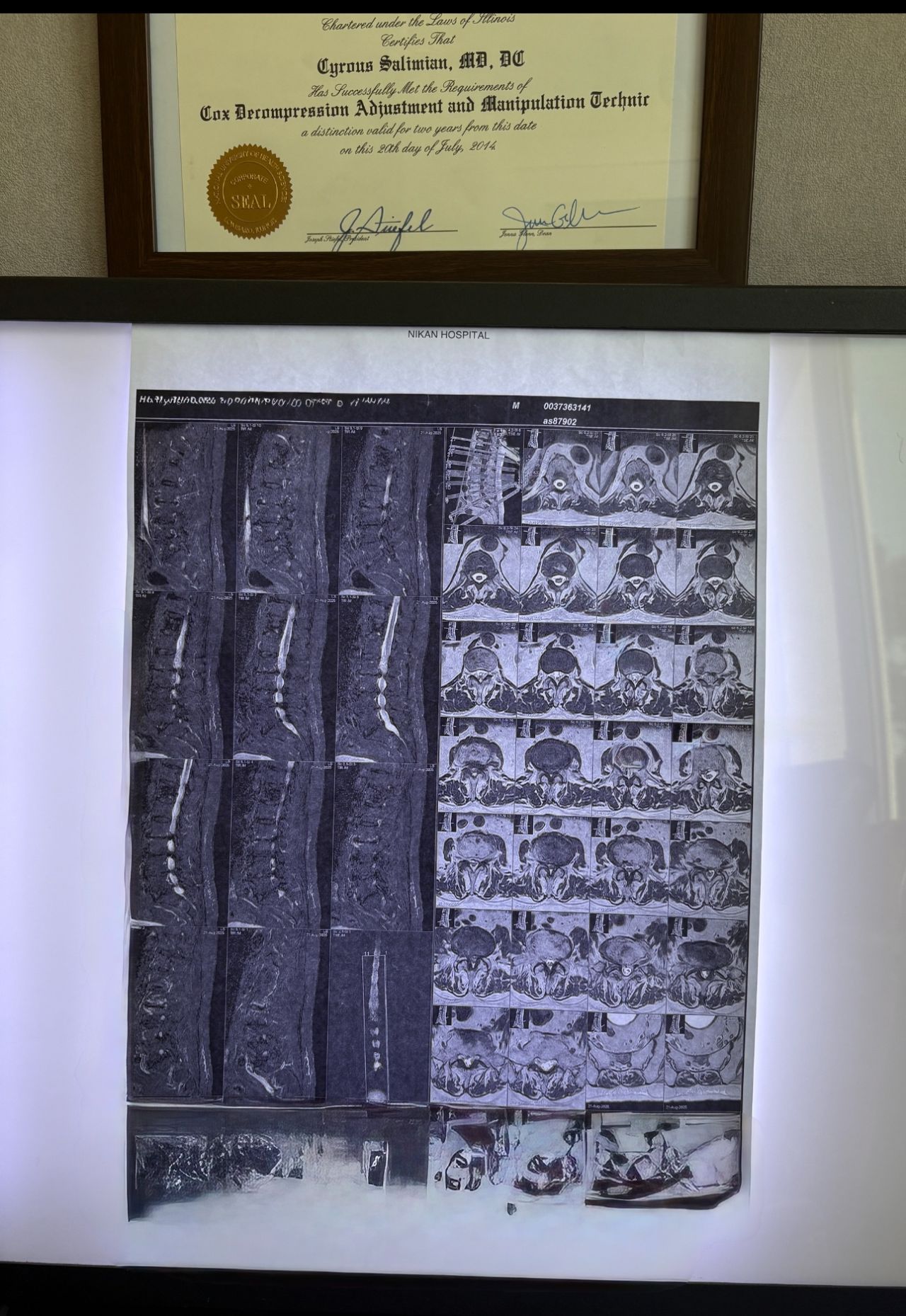
A 65-year-old patient presented to my office 20 days ago with right hip/gluteal pain, mainly occurring after walking approximately 200 meters. He also reported right shoulder and neck pain.
On examination, the right shoulder range of motion was normal. However, cervical spine (C/S) range of motion was severely restricted by about 80% in all directions. There was severe right C5–C7 dysfunction. Neurological examination revealed a positive right-sided Hoffman’s sign, unremarkable Babinski sign, and bilateral L4 deep tendon reflexes graded 1+. On palpation of the lumbar spine, step defects were noted. Right hip examination was otherwise normal.
Cervical and lumbar MRI, dynamic lumbosacral X-rays, and EMG/NCV of the lower limbs were ordered. The patient brought all results today (August 18, 2025).
Request:
Please review his MRI and X-ray findings. Based on these, what are your differential diagnoses, final diagnosis, and plan of management (POM)?
Case 26
A 74-year-old female patient presented to my office yesterday with right leg pain. She has a history of left breast cancer with a lump, for which she received chemotherapy and radiotherapy 24 years ago, but no lumpectomy. She visited her oncologist one month ago and was told that everything was fine.
Please review her MRI and provide your findings, differential diagnoses, and suggested management plan.
Case 27
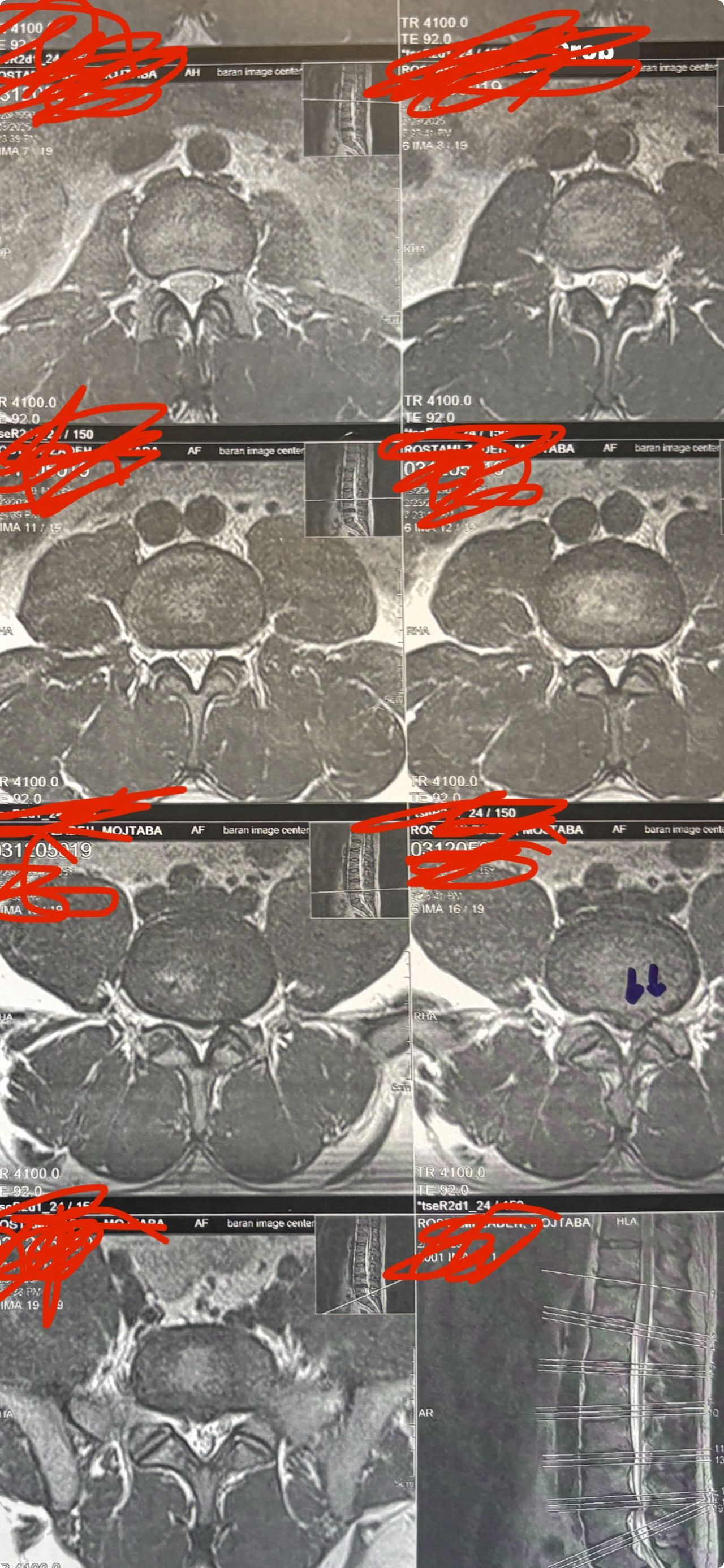
40 yrs old male patient was seen at my clinic on Aug 11 due to chronic LBP and L leg radicular pain in sitting no neurological signs
I will treat him by Cox and DTS and acupuncture
No adjustments but i prefer to have emg/ncv of his lower limbs first to get sure about any active and ongoing or chronic axol loss
If anyone has any suggestions in his further initial assessment and plan of managementant and his precise reevaluation during treatment( if you start to give treatment to this patient how often you have to reevaluate this patient? If you see neurological deficits are showing up or progressive neurological deficits are happening what will you do?)
If during treatment patient’s pain suddenly in 1-2 days disappears what could be the reason?
please bring it up
A good chiropractor is the one who can have proper/correct selection of their patient at the beginning and properly can handle and change/manage the patient’s POM
Case 28
Spinal MRI without injection Before any actual adjustment or manipulation in A Case for the safety of the patient not based on the buget of the paying third party
⸻
Abstract
A 56-year-old male with chronic low back pain and mild cervical tightness was evaluated for chiropractic care. Lumbar MRI revealed L4–L5 degeneration. Cervical exam showed facet dysfunction without neurological deficits. Although clinically eligible for cervical manipulation without mri ( according to the guidelines) C/S treatment was delayed until a cervical MRI was obtained. Initial insurance denial for mri like spinal/cervical mri is so common
This case supports the routine use of spinal MRI before any manipulation
Making
Insurance or MOH guidelines should be based on the patient’s safety first not their own budget
Third parties or doctors should have complete transparency in their actions and tell patients your mri is not covered by them due to lack of enough budget
⸻
Introduction
Chiropractors in patients with lumbar complaints often address cervical adjustments concurrently. While cervical manipulation is widely used, it carries rare but serious risks, especially in older patients.
Pre-treatment MRI can help to find thosewhyare at risks but it is often covered by insurance providing their own criteria and in canada by MOH guidelines
⸻
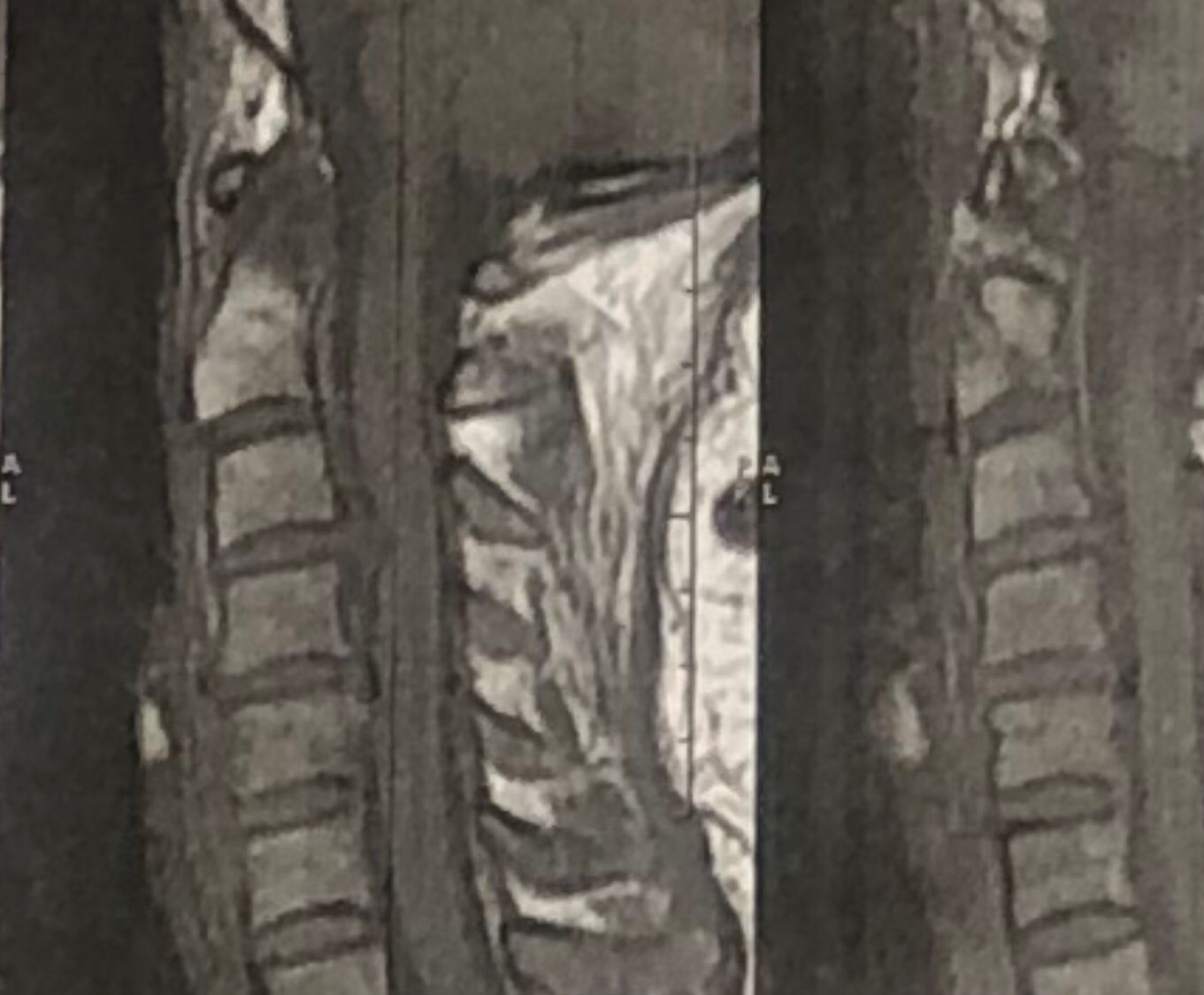
Case Report
A 56-year-old man presented with chronic low back pain and mild neck stiffness. Lumbar MRI confirmed disc degeneration. In cervical MRI C5-6 Cervical extrusion with cervical cord compression is seen
And neurological exams were normal for cervical spine
therefore according to the cervical mri no cervical treatment was rendered to his neck
Insurance initially denies paying for MRI but patients can pay themselves if they want to get neck adjustment
.cervical adjusting was not rendered and patient was referred to the neurosurgeon
⸻
Conclusion
Spinal Mri should be done on all patients before adjustment Insurance decisions and their guidelines must be transparent and ethically aligned with patient safety.
Case 29
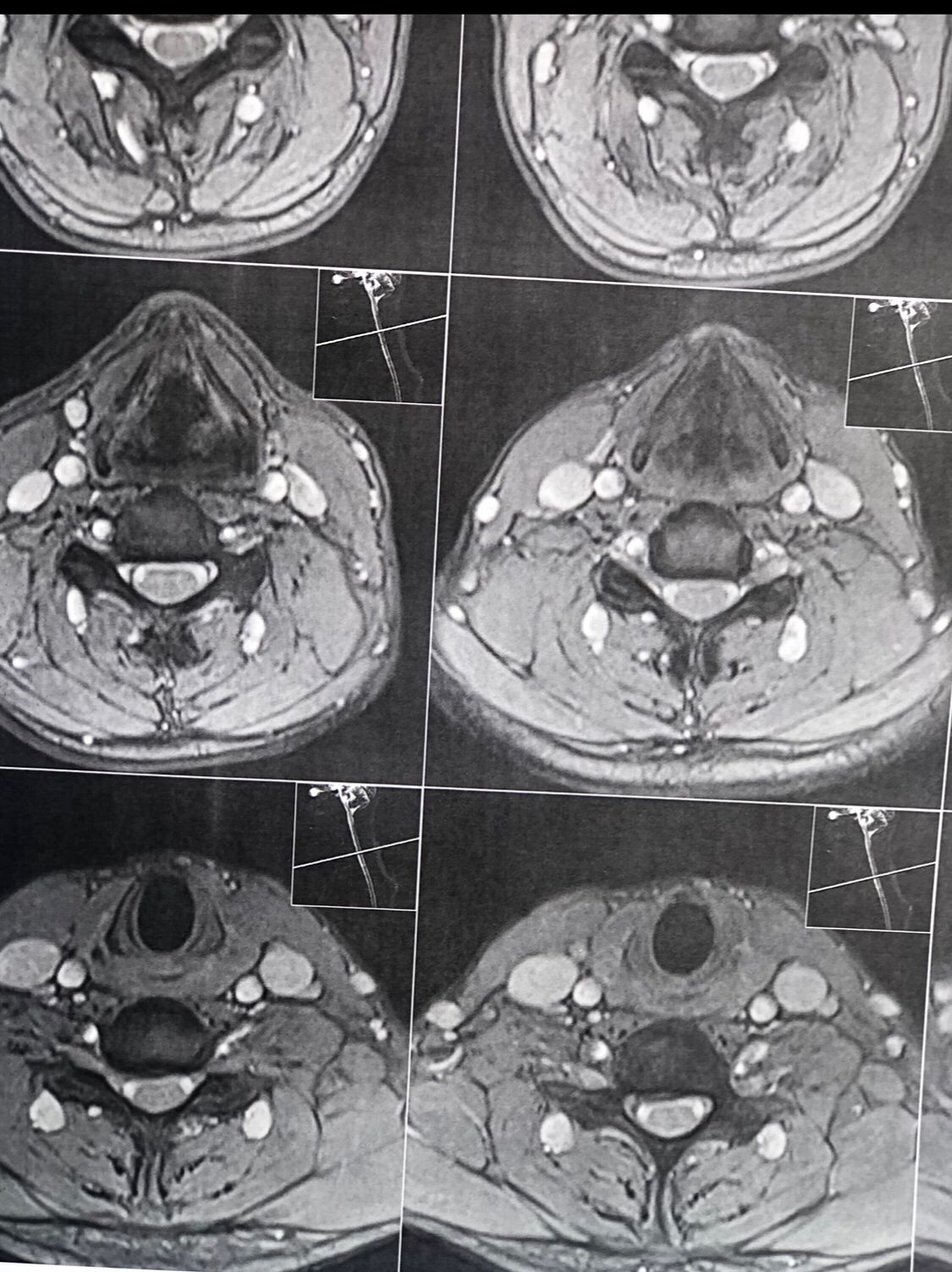
A 64-year-old male patient was referred to my clinic by a well-known neurosurgeon (Oct 2025) for evaluation and management of right-sided sciatic pain. The onset followed an incident in which his 18-year-old grandson accidentally pulled his leg. Relevant medical documents were reviewed and attached. He just has controled DM
On presentation, the patient denied any cervical pain. Nevertheless, as part of my routine examination protocol, a comprehensive cervical assessment was performed, including chiropractic, orthopedic, and neurological evaluations. Cervical range of motion was markedly restricted, and chiropractic motion and static palpations revealed hypertrophic pillar segments and multiple severe Facets restrictions .There were no upper motor neuron (UMN) signs at all noted during the examination.
Investigations and Management;
A cervical and thoracic MRI was requested, and lumbar treatment was initiated for his sciatic symptoms. The patient was also advised to follow up with his neurosurgeon regarding the cervical findings.in his mri a large hydronephrosis was noticed and For his large hydronephrosis he was asked to see a nephrologist ( he mentioned he had ESWL for kidney stone few years ago)
Upon further discussion with the patient after reviewing his cervical MRI with him , the patient mentioned that he had previously fallen from a three-story building, sustaining ankle fractures at that time.after seeing his cervical mri the possibility of C4,5, and possibly retrolisthesis of C5 was considered and CT scan from C/S and dynamic cervical x ray was requested
Discussion
Although the patient was asymptomatic from a cervical standpoint, MRI findings demonstrated cervical cord severe compression and possible mild edema and early myelomalacia. Based on these findings, I believe that cervical decompression surgery should be considered.
While some neurologists and chiropractors may defer intervention in the absence of overt clinical symptoms, in this case, early surgical decompression appears justified. Waiting for neurological deficits—such as gait imbalance, coordination difficulties, or gastrointestinal/genitourinary dysfunction—may result in irreversible spinal cord injury, as these deficits often persist even after surgical decompression.
Considering the patient’s age and progressive degenerative changes, including degenerative disc disease (DDD) and degenerative joint disease (DJD), delaying surgery could further increase the risks associated with operative morbidity and mortality. Keep in mind all kind of manipulation on his neck is absolutely contraindicated
Conclusion;
Early identification and management of clinically silent cervical cord compression with MRI evidence with or without myelomalacia may prevent irreversible neurological deterioration in future.on the other hand he has to take care of his kidney seriously
I welcome interprofessional opinions and discussion regarding the optimal management strategy for this patient’s cervical spine pathology, particularly concerning the timing and indications for surgical decompression in the absence of overt cervical symptoms.
Case 30
A 70-year-old male patient presented to my clinic two weeks ago. While he was in the waiting area, he gradually lost consciousness. We immediately laid him on the floor; his pulse was very weak, but his condition gradually returned to normal. Emergency services (911) were called. He was evaluated on-site, and no acute cardiac or neurological abnormalities were identified.
After approximately one hour of assessment by both our team and the emergency responders, he was able to walk into my examination room for his initial visit.
He reported experiencing gait imbalance for several months, along with numbness in his legs. On examination, upper motor neuron signs were present, including bilateral upgoing Babinski signs, positive Hoffman signs, and hyperreflexia with L4 deep tendon reflexes rated at 4+.
Please describe your recommended management plan for this patient.